Hey reader,
as promised - another round of sky-high blogging to complete the circle.
I'm on the plane back from the Windy City after a long morning of finishing up packing, sweeping carpet floor with my broom (a vacuum was not among the things I had bought from Target) and giving heaps of stuff away to one of the Germans and the sociologist. Over the course of just one hour this morning, pretty much everything except one can of olives found a new home and I had to throw away very little.
I was just about done tidying up and getting ready to go around 12pm, Nema, whose flight departed around 3pm was long gone by then. The bad thing about that was that she was getting a ride with one of her roommates to the airport which was just so much more convenient than the one and a half hours of one bus and two train rides with my suitcase and two bags in the summer Chicago heat I was looking forward to. But I had missed that ride, so there I was, dropping off my keys and my laundry card at the graduate student housing office mailbox. Back across the street, there was actually a bus coming.
So far so good - but the driver warned us not to come in because her bus had been breaking down all morning and she couldn't guarantee to take us anywhere. That veered off me plus another young guy with a big bag who asked whether I was going to the airport.
Yeah, I was.
- Me too, been waiting for a bus for 15 minutes and now this, I'll have to take my car. Want a ride?
AWESOME!
- Can you watch my bag while I get the car?
You betcha, dude! Were things shaping up to repeat my incredible traveling luck from the way here?
Not quite!
We found out rather quickly that we had two different airports in mind. Rats. He wasn't going to O'Hare. BUT, he saved me the bus ride by dropping me off at the green line, which did bring me a short distance but otherwise long bus ride towards O'Hare.
The rest went rather smoothly except for me having to find out the hard way after lugging my baggage across the terminal to the Lufthansa check-in that this flight was going to be handled by United again after all.
And this time the bastards actually did make me sit with the cheap crowd. I miss the attention.
But they do have individual TV screens even here now so who am I to complain.
I still don't quite feel like writing the overall evaluation of the trip here so you'll have to wait a little longer for that while I pop in an episode of Battlestar Galactica now. I'm never able to sleep on these flights anyway.
Blog to you later.
Sunday, June 3, 2007
Thursday, May 31, 2007
Good bye.
So strange.
After parting with my team today, only saying a proper goodbye to the attending because I'll see the fellow again tomorrow to pick up a letter she's writing for me I went to get the signed confirmation that I'll need for my medschool and turn in my pager. After that, I went up to Brainy's office to say goodbye to her, arriving at the same time as the heart failure team that wanted to round. But Brainy was on the phone anyway and they let me trade goodbyes with her before they started.
It was only after I left her office that I started feeling sad. Like they always say .. you never know what you have until you lose it. Working here was fun. I've pretty much decided not to come to the United States permanently - but that certainly wasn't for the work environment.
Walking down those halls in my terribly ugly short white coat towards the exit for the very last time even choked a heartless person like me up a little. And as if in agreement, a hot summer rain had started just around this time.
After parting with my team today, only saying a proper goodbye to the attending because I'll see the fellow again tomorrow to pick up a letter she's writing for me I went to get the signed confirmation that I'll need for my medschool and turn in my pager. After that, I went up to Brainy's office to say goodbye to her, arriving at the same time as the heart failure team that wanted to round. But Brainy was on the phone anyway and they let me trade goodbyes with her before they started.
It was only after I left her office that I started feeling sad. Like they always say .. you never know what you have until you lose it. Working here was fun. I've pretty much decided not to come to the United States permanently - but that certainly wasn't for the work environment.
Walking down those halls in my terribly ugly short white coat towards the exit for the very last time even choked a heartless person like me up a little. And as if in agreement, a hot summer rain had started just around this time.
Wednesday, May 30, 2007
Excitement
The day started out as usual, went up to A700 to get breakfast after getting up to speed with my patients from the past days. I hung out with some Germans and listened to morning report, which was about an interesting case of a 28-year-old pregnant patient that presented to two different ERs with a cough, one of those ERs being ours, both of those ERs making a chest x-ray (yes, on a pregnant patient!) and sending the patient home, both ERs calling the patient back into the ER after having taken a second look at the x-ray. After they did a CT at the U of Chicago (yes, patient still pregnant .. at least pre-CT ..) they found her to have sarcoidosis.
But that was not the exciting part. Neither was my stroll afterwards, at around 11am to the cardiology fellows' room to check in with Missy. She said that she hadn't gotten a consult yet and with a smile on her face offered that if there wasn't a consult by noon, I should go home (the weather today is what other people would call gorgeous .. I actually liked the mostly air-conditioned interior of the hospital at that point). Even when she said that though, I knew that wasn't going to help her karma. It's those days where the morning seems like nothing's going to happen that come back to bite you in the ass. Which was good. I wanted to do consults. That's what I'm here for.
So I left the fellows' room thoroughly expecting the page that came half an hour later about a patient in one of the surgical ICUs. She had received a left lung transplant yesterday. Somehow I still have a high level of respect for lung transplants. But the way they have simply extubated the patient this morning, just about 12 hours after surgery and the way Missy would just send a foreign med student that's still coughing once in a while to see this highly immunosuppressed patient breathing with someone else's lung for a few hours now started wearing down this respect.
Anyway, I went up to that ICU and spent the rest of the time until noon getting started with the consult, jotting down her history and deciphering some of the surgical (i.e. minimal and cryptic) notes of the past days. The reason we were called was that the anesthesiologist who did the intraoperative transesophageal echo found severe mitral regurgitation. I looked at the pre-transplant workup and found a right heart catheter from just a few months ago numbering her pulmonary capillary wedge pressure at 1 mmHg which all but rules out any mitral regurgitation back then. That means if she had MR now, it would have to be rather acute. So I did check in on the patient - who was doing remarkably well, obviously having pain in her chest on day one post surgery but was very lucid and pleasant to talk to - before going back to A700 for lunch and an interesting infectious disease conference on endocarditis.
I had meant to go back to finish the consult about half an hour into the conference, after having enjoyed the excellent free Potbelly lunch. But the presenter from ID did such a great job presenting that I stayed until the end at about 1pm. So that's when I went back to the ICU.
After settling down again with the patient's charts (because they have two on ICU) I happily scribbled away at my consult sheet when the surgical resident from the primary team asked me whether I was from cardiology.
Sure.
- Oh good. Cardiac enzymes just came back positive. Did you see the EKGs?
There were EKGs? You drew enzymes? What's going on?
- Oh the EKGs are not in the charts, huh. Let me see if I can track down the nurse to find them.
And off she went after the nurse to get the EKGs. While she did that, I brought up the patient's labs on oacis and sure enough, she had had cardiac enzymes drawn this morning at 2am and again around noon. The latter ones had just come back positive with a troponin of 0.26 - with the 2am ones already at 0.16. CK-MB ratio was also mildly positive on both.
Just about after I had found this out, the nurse came around with two EKG's from the patient. They had almost identical time stamps to the two sets of cardiac enzymes, 2am and noon. The 2am EKG looked normal enough. The noon one had pretty impressive ST elevations in the inferior and lateral leads, yet not in the anterior ones. With scaredly-widened eyes I looked up to the nurse (the surgical resident had apparently taken off again) and asked her if the patient had chest pain with this.
Of course the patient had chest pain.
Duh. She had had her left lung replaced yesterday.
So this patient had chest pain, positive cardiac enzymes, a new onset of localized ST-elevations on a day after major surgery and I seemed the only one freaking out about this. That couldn't stay that way, so I paged Missy with a text page saying just that - something along the lines of "pt has cp (confounded by surgery), + enzymes and ST-elev. I think you". Apparently, as I later learned, I must have sent the page before I was done writing it because it ended in the middle of a sentence and before I gave a call-back number or my own pager number to identify who sent the page. This may have happened because I was showing Jen, who happened to be there, the EKGs and running to the patient's cubicle to look at the vitals on the monitor while writing parts of the page. Which was why Missy never called back.
Jen was seeing another patient and had come over to chat so I showed her those EKGs. Being a nephrologist, she said she hadn't been reading EKGs in a while but agreed this together with positive enzymes was likely to be either pericarditis or an acute myocardial infarction.
I knew this had to happen on a day that Missy wants to send me home at noon. With Missy not answering her page (which she couldn't as I only found out later) I went to the most extreme measures, came into the patient's cubicle and talked to her. And when asked about it specifically, she'd say that she had no pain in her chest - unless she moved.
Phew.
Her vitals were stable, on two pressors admittedly. But stable, and the patient had no chest pain at rest. Then again, she had a high epidural. I still didn't quite understand why I was the only one worrying there. I was about to send another page to Missy, when she came into the ICU around 2pm. She showed me the botched-up page that I apparently had sent and said that she had checked up on the other patients on the service that were a little more likely to be having acute MIs than mine not knowing where or who the page came from.
Oops.
So I gave her a quick run down on the patient's story and came to the enzyme and EKG part rather quickly. She was similarly relieved by the fact that the patient had no chest pain and a decent blood pressure of 100/60 and also pointed out the PQ depression hinted at in some leads that would make pericarditis more likely. But she asked for another EKG nonetheless, since the one we had was already two and a half hours old by then.
That's when the attending called to go start rounding in ten minutes. Missy had gotten another consult in the meantime (karma's a bitch), so we went down to that other ICU to at least grab that person's EKGs before meeting the attending in the workroom.
We relayed the most pertinent information about our patients to him upfront but he'd of course as always want to look at a maximum amount of "pictures" (read: imaging studies) on all the patients we were going to see. So that took a while and afterwards, when deciding which patient to see first, we went to see Missy's patient. She wasn't as critical as the patient in ICU but geographically closer. Guess that's what you get for being on a regular floor.
Afterwards, we finally went to see the freshly transplanted lady at around 3:45pm but we were apparently just in time, the tech was in the process of writing my patient's third EKG for the day. While we were kind of aimlessly standing around waiting for her to get done, I saw the first Dr. Cart being initiated in front of my eyes.
No, it wasn't on my patient.
I was leaning on the ICU's coordinating clerk's desk which was just a few steps outside of another patient's cubicle. Anyone who's ever been on an ICU knows they are noisy places with ubiquitous and incessant beeping coming from somewhere or other around the clock. There's so much of it you get used to it and you don't even consciously perceive it anymore.
Except for a few kinds of beeping - those ones where the monitor actually means business.
And this was one of them.
When I looked up from the desk into the cubicle right across from me, the blue and red lights on top of the actual screen of the monitor flashed alternatingly, while the screen read multiple wide-complex QRS's in rapid succession - this was ventricular tachycardia. Inside the room were a nurse and a relative - the nurse poked her head out of the cubicle and yelled for the crash cart, while the relative gave a yelp and started to cry, before storming out of the cubicle, seemingly to make way for the influx of the ICU staff that was about to happen. While the nurse that was originally there opened the hinged glass walls on the front of the cubicle another nurse flattened the patient's bed before the rest of the ICU people including my consult team had the patient's bed surrounded and all I could see from the desk was the monitor.
That didn't look good though. The VT had apparently subsided and reverted into some kind of slow narrow-complex rhythm, maybe sinus brady, maybe junctional, couldn't tell from where I was standing. I did see the blood pressure from the arterial line around 60/40 and occasionally dropping further though. I knew nothing of the patient's history but her future seemed increasingly in jeopardy. At this point someone yelled to "call a Dr. Cart", which the ICU clerk right next to me did. Just moments later, the overhead public announcement system made another all-too-familiar overhead page to "Dr. Cart", this time calling to the bed I was standing at.
They started compressions right around that time and since there wasn't going to be much I'd be doing with the code, I grabbed the new EKG of my patient from the tech and compared it to the two other ones of that day. And I must have had that wide-eyed look of fear again - not only did her ST-elevations get worse in the lateral leads, I hadn't before noticed that she had had a solid 1mV R in lead III at 2am, that had become isoelectric at noon. Already then there wouldn't have been much blaming this on lead placement, since these are limb leads and the P axis did not change. But now, on this EKG close to four hours later, this lady did not have an R in III anymore, it was a 1mV Q.
I showed the EKGs to my team who were now more on the outer rim of the Dr. Cart crowd and the attending had an interesting way of putting it .. "oh no. She is losing voltage." Finally, things became more hectic with this patient and the attending told the patient that he'd say her odds were about 60% of having a heart attack and 40% of just having pericarditis and that he'd suggest they do a cath right away.
Outside the room, Missy voiced her concerns about this patient. She wasn't as sure about this patient having an acute MI as the attending and she was making a good point. The patient just wasn't symptomatic enough. Blood pressure was stable on the pressors and she just didn't have any pain. She didn't quite convince the attending though. He agreed that the clinical picture was underwhelming for this amount of EKG changes and that pericarditis was a more likely explanation - so the odds were maybe 40 to 60 or even 20 to 80. But even with only a 20% chance of this person having a huge infarction - can you afford not to cath her?
While the attending was talking to the primary team I followed Missy to the cath lab, where she was about to inform their people about the patient and show them the EKGs. On the way, she made another good point, being that the patient was severely medically immunocompromised and about to be wheeled through the hospital to the cath lab where someone would be poking wires around her freshly operated-on mediastinum. The cath wasn't a benign procedure.
This was a really tough decision to make.
Missy said that she was "only a fellow" and was afraid to be "too cavalier" in her opinion to rather "ride this one out" rather than sending the patient to cath. I disagreed in so far as I didn't find it cavalier to be seeing the whole picture and to be afraid the patient could die of overwhelming infection with totally clean coronary arteries just a week from now if we do wheel her to the cath lab.
When we returned to the ICU, though, the decision was basically taken off our hands. The attending cardiothoracic surgeon of the primary team answered his page and talked to our attending. Two new pieces of information prevented the cath - for one thing no one among all those people involved in this so far had been privy to the fact that during her transplant surgery, not only the pericardium but also the left atrium had been cut open for the anastomosis of the pulmonary veins. That was a good explanation of the cardiac enzymes and pericarditis on EKG and made them even more likely, still didn't quite rule out infarction though. However, the other piece of information was that the surgical attending expressly forbid us to use aspirin, clopidogrel or heparin even if we did find something on cath. The only thing he would let us put her on among the usual MI medication was a beta-blocker, which she got. With all those meds out of the picture and stents therefore not being an option there wouldn't be much point in a cath anyway, with angioplasty being unlikely to change much.
So unless a third set of enzymes would come back exceedingly high, there'd be no cath on her today. This will be something interesting to follow up on tomorrow.
After getting home this afternoon I met the sociologist again and he took me to one of the two places in Hyde Park to go out in, as I learned from him there. And apparently, he now also is a reader of this blog so I cannot say any more evil things about him. Rats.
During the several hours we talked I learned among many other things that the University, owning a significant portion of Hyde Park, actually and actively prevented more leisurely (read: alcohol-dispensing) places to open up around campus.
Shame on them!
Look, it's half an hour into Thursday already - my very final day in the U of C hospital. Time to finally write that summary report I've been promising, isn't it.
Well if you're waiting for that, just hope that no more exciting days come in the way.
And tomorrow afternoon the entire Chicago gang is invited to barbecue at CS's place.
I may just end up blogging the retrospective report from Germany - or maybe the plane. Some sky-high-blogging for the perfect circle. See! It did pay off to have read this whole thing for that beautiful sense of closure, right? RIGHT?
OK never mind, I should sleep.
Blog to you later.
But that was not the exciting part. Neither was my stroll afterwards, at around 11am to the cardiology fellows' room to check in with Missy. She said that she hadn't gotten a consult yet and with a smile on her face offered that if there wasn't a consult by noon, I should go home (the weather today is what other people would call gorgeous .. I actually liked the mostly air-conditioned interior of the hospital at that point). Even when she said that though, I knew that wasn't going to help her karma. It's those days where the morning seems like nothing's going to happen that come back to bite you in the ass. Which was good. I wanted to do consults. That's what I'm here for.
So I left the fellows' room thoroughly expecting the page that came half an hour later about a patient in one of the surgical ICUs. She had received a left lung transplant yesterday. Somehow I still have a high level of respect for lung transplants. But the way they have simply extubated the patient this morning, just about 12 hours after surgery and the way Missy would just send a foreign med student that's still coughing once in a while to see this highly immunosuppressed patient breathing with someone else's lung for a few hours now started wearing down this respect.
Anyway, I went up to that ICU and spent the rest of the time until noon getting started with the consult, jotting down her history and deciphering some of the surgical (i.e. minimal and cryptic) notes of the past days. The reason we were called was that the anesthesiologist who did the intraoperative transesophageal echo found severe mitral regurgitation. I looked at the pre-transplant workup and found a right heart catheter from just a few months ago numbering her pulmonary capillary wedge pressure at 1 mmHg which all but rules out any mitral regurgitation back then. That means if she had MR now, it would have to be rather acute. So I did check in on the patient - who was doing remarkably well, obviously having pain in her chest on day one post surgery but was very lucid and pleasant to talk to - before going back to A700 for lunch and an interesting infectious disease conference on endocarditis.
I had meant to go back to finish the consult about half an hour into the conference, after having enjoyed the excellent free Potbelly lunch. But the presenter from ID did such a great job presenting that I stayed until the end at about 1pm. So that's when I went back to the ICU.
After settling down again with the patient's charts (because they have two on ICU) I happily scribbled away at my consult sheet when the surgical resident from the primary team asked me whether I was from cardiology.
Sure.
- Oh good. Cardiac enzymes just came back positive. Did you see the EKGs?
There were EKGs? You drew enzymes? What's going on?
- Oh the EKGs are not in the charts, huh. Let me see if I can track down the nurse to find them.
And off she went after the nurse to get the EKGs. While she did that, I brought up the patient's labs on oacis and sure enough, she had had cardiac enzymes drawn this morning at 2am and again around noon. The latter ones had just come back positive with a troponin of 0.26 - with the 2am ones already at 0.16. CK-MB ratio was also mildly positive on both.
Just about after I had found this out, the nurse came around with two EKG's from the patient. They had almost identical time stamps to the two sets of cardiac enzymes, 2am and noon. The 2am EKG looked normal enough. The noon one had pretty impressive ST elevations in the inferior and lateral leads, yet not in the anterior ones. With scaredly-widened eyes I looked up to the nurse (the surgical resident had apparently taken off again) and asked her if the patient had chest pain with this.
Of course the patient had chest pain.
Duh. She had had her left lung replaced yesterday.
So this patient had chest pain, positive cardiac enzymes, a new onset of localized ST-elevations on a day after major surgery and I seemed the only one freaking out about this. That couldn't stay that way, so I paged Missy with a text page saying just that - something along the lines of "pt has cp (confounded by surgery), + enzymes and ST-elev. I think you". Apparently, as I later learned, I must have sent the page before I was done writing it because it ended in the middle of a sentence and before I gave a call-back number or my own pager number to identify who sent the page. This may have happened because I was showing Jen, who happened to be there, the EKGs and running to the patient's cubicle to look at the vitals on the monitor while writing parts of the page. Which was why Missy never called back.
Jen was seeing another patient and had come over to chat so I showed her those EKGs. Being a nephrologist, she said she hadn't been reading EKGs in a while but agreed this together with positive enzymes was likely to be either pericarditis or an acute myocardial infarction.
I knew this had to happen on a day that Missy wants to send me home at noon. With Missy not answering her page (which she couldn't as I only found out later) I went to the most extreme measures, came into the patient's cubicle and talked to her. And when asked about it specifically, she'd say that she had no pain in her chest - unless she moved.
Phew.
Her vitals were stable, on two pressors admittedly. But stable, and the patient had no chest pain at rest. Then again, she had a high epidural. I still didn't quite understand why I was the only one worrying there. I was about to send another page to Missy, when she came into the ICU around 2pm. She showed me the botched-up page that I apparently had sent and said that she had checked up on the other patients on the service that were a little more likely to be having acute MIs than mine not knowing where or who the page came from.
Oops.
So I gave her a quick run down on the patient's story and came to the enzyme and EKG part rather quickly. She was similarly relieved by the fact that the patient had no chest pain and a decent blood pressure of 100/60 and also pointed out the PQ depression hinted at in some leads that would make pericarditis more likely. But she asked for another EKG nonetheless, since the one we had was already two and a half hours old by then.
That's when the attending called to go start rounding in ten minutes. Missy had gotten another consult in the meantime (karma's a bitch), so we went down to that other ICU to at least grab that person's EKGs before meeting the attending in the workroom.
We relayed the most pertinent information about our patients to him upfront but he'd of course as always want to look at a maximum amount of "pictures" (read: imaging studies) on all the patients we were going to see. So that took a while and afterwards, when deciding which patient to see first, we went to see Missy's patient. She wasn't as critical as the patient in ICU but geographically closer. Guess that's what you get for being on a regular floor.
Afterwards, we finally went to see the freshly transplanted lady at around 3:45pm but we were apparently just in time, the tech was in the process of writing my patient's third EKG for the day. While we were kind of aimlessly standing around waiting for her to get done, I saw the first Dr. Cart being initiated in front of my eyes.
No, it wasn't on my patient.
I was leaning on the ICU's coordinating clerk's desk which was just a few steps outside of another patient's cubicle. Anyone who's ever been on an ICU knows they are noisy places with ubiquitous and incessant beeping coming from somewhere or other around the clock. There's so much of it you get used to it and you don't even consciously perceive it anymore.
Except for a few kinds of beeping - those ones where the monitor actually means business.
And this was one of them.
When I looked up from the desk into the cubicle right across from me, the blue and red lights on top of the actual screen of the monitor flashed alternatingly, while the screen read multiple wide-complex QRS's in rapid succession - this was ventricular tachycardia. Inside the room were a nurse and a relative - the nurse poked her head out of the cubicle and yelled for the crash cart, while the relative gave a yelp and started to cry, before storming out of the cubicle, seemingly to make way for the influx of the ICU staff that was about to happen. While the nurse that was originally there opened the hinged glass walls on the front of the cubicle another nurse flattened the patient's bed before the rest of the ICU people including my consult team had the patient's bed surrounded and all I could see from the desk was the monitor.
That didn't look good though. The VT had apparently subsided and reverted into some kind of slow narrow-complex rhythm, maybe sinus brady, maybe junctional, couldn't tell from where I was standing. I did see the blood pressure from the arterial line around 60/40 and occasionally dropping further though. I knew nothing of the patient's history but her future seemed increasingly in jeopardy. At this point someone yelled to "call a Dr. Cart", which the ICU clerk right next to me did. Just moments later, the overhead public announcement system made another all-too-familiar overhead page to "Dr. Cart", this time calling to the bed I was standing at.
They started compressions right around that time and since there wasn't going to be much I'd be doing with the code, I grabbed the new EKG of my patient from the tech and compared it to the two other ones of that day. And I must have had that wide-eyed look of fear again - not only did her ST-elevations get worse in the lateral leads, I hadn't before noticed that she had had a solid 1mV R in lead III at 2am, that had become isoelectric at noon. Already then there wouldn't have been much blaming this on lead placement, since these are limb leads and the P axis did not change. But now, on this EKG close to four hours later, this lady did not have an R in III anymore, it was a 1mV Q.
I showed the EKGs to my team who were now more on the outer rim of the Dr. Cart crowd and the attending had an interesting way of putting it .. "oh no. She is losing voltage." Finally, things became more hectic with this patient and the attending told the patient that he'd say her odds were about 60% of having a heart attack and 40% of just having pericarditis and that he'd suggest they do a cath right away.
Outside the room, Missy voiced her concerns about this patient. She wasn't as sure about this patient having an acute MI as the attending and she was making a good point. The patient just wasn't symptomatic enough. Blood pressure was stable on the pressors and she just didn't have any pain. She didn't quite convince the attending though. He agreed that the clinical picture was underwhelming for this amount of EKG changes and that pericarditis was a more likely explanation - so the odds were maybe 40 to 60 or even 20 to 80. But even with only a 20% chance of this person having a huge infarction - can you afford not to cath her?
While the attending was talking to the primary team I followed Missy to the cath lab, where she was about to inform their people about the patient and show them the EKGs. On the way, she made another good point, being that the patient was severely medically immunocompromised and about to be wheeled through the hospital to the cath lab where someone would be poking wires around her freshly operated-on mediastinum. The cath wasn't a benign procedure.
This was a really tough decision to make.
Missy said that she was "only a fellow" and was afraid to be "too cavalier" in her opinion to rather "ride this one out" rather than sending the patient to cath. I disagreed in so far as I didn't find it cavalier to be seeing the whole picture and to be afraid the patient could die of overwhelming infection with totally clean coronary arteries just a week from now if we do wheel her to the cath lab.
When we returned to the ICU, though, the decision was basically taken off our hands. The attending cardiothoracic surgeon of the primary team answered his page and talked to our attending. Two new pieces of information prevented the cath - for one thing no one among all those people involved in this so far had been privy to the fact that during her transplant surgery, not only the pericardium but also the left atrium had been cut open for the anastomosis of the pulmonary veins. That was a good explanation of the cardiac enzymes and pericarditis on EKG and made them even more likely, still didn't quite rule out infarction though. However, the other piece of information was that the surgical attending expressly forbid us to use aspirin, clopidogrel or heparin even if we did find something on cath. The only thing he would let us put her on among the usual MI medication was a beta-blocker, which she got. With all those meds out of the picture and stents therefore not being an option there wouldn't be much point in a cath anyway, with angioplasty being unlikely to change much.
So unless a third set of enzymes would come back exceedingly high, there'd be no cath on her today. This will be something interesting to follow up on tomorrow.
After getting home this afternoon I met the sociologist again and he took me to one of the two places in Hyde Park to go out in, as I learned from him there. And apparently, he now also is a reader of this blog so I cannot say any more evil things about him. Rats.
During the several hours we talked I learned among many other things that the University, owning a significant portion of Hyde Park, actually and actively prevented more leisurely (read: alcohol-dispensing) places to open up around campus.
Shame on them!
Look, it's half an hour into Thursday already - my very final day in the U of C hospital. Time to finally write that summary report I've been promising, isn't it.
Well if you're waiting for that, just hope that no more exciting days come in the way.
And tomorrow afternoon the entire Chicago gang is invited to barbecue at CS's place.
I may just end up blogging the retrospective report from Germany - or maybe the plane. Some sky-high-blogging for the perfect circle. See! It did pay off to have read this whole thing for that beautiful sense of closure, right? RIGHT?
OK never mind, I should sleep.
Blog to you later.
Thursday, May 24, 2007
Yes I am
still alive and kicking. I've been sick over the weekend and I actually took Monday off, partly because it's just annoying to be blowing your nose every few seconds but mainly because I just don't want to be responsible for a ton of ID consults on patients and staff just about a week from now.
When I did work last week though I kept surprising myself by having a lot of answers during discussions and rounds. Especially with this one attending that "rounded" with us at his desk (much like the very first renal attending). He was a stud, appeared very young and overflowing with confidence, obviously was working out and judging from the pictures in his office he had his trophy wife tucked away (OK now I'm going a bit too far). Obviously, he was knowledgeable - you don't become an attending for nothing here. So while rounding in his office with Missy and the female intern on the team as soon as I started presenting my patient he'd say that we were going to have a "guy discussion" from now on, which apparently meant that we'd leave political correctness and etiquette aside - which was very refreshing and fun.
I didn't see much of that attending - he only filled in for the regular one that day. But from what I have experienced and heard about him I guess he is an extremely - maybe overly - confident guy that will be your best friend and not worry too much about taking care of patients himself as long as everything goes well. Apparently though, the yelling starts if ever things go south and he may ultimately be made responsible for something he should have taken more care of. So he's a nice, extremely suave and cool guy and he does seem to know his stuff but I still wouldn't want him as my attending - whether I'm on his team OR his patient.
But like I said, my experience with him was brief.
Over the weekend, like I said, I was sick and didn't do much except raiding the pharmacy for cold medication that turned out to be placebos for the most part - including the facial tissues. The stuff they sell there really is a very bad joke. Unless you use at least three of those tissues at once you might as well blow your nose into your hand directly. While at home with my headache I did get started typing down an exposé of the mentoring project the Chicago group has been working on. As of last night, it was up to 10 typed pages, I'm still waiting for the rest of the group to read it and sign off on it so we can pass the first drafts on to the good people in Boston and Munich. But I have high hopes for the next project meeting tonight at 6pm.
In other news, the service has been very light these past days and I was able to attend a lot of conferences today. Among them was a so-called "code review" where they discussed a few of the Dr. Cart (=cardiac arrest) calls that had happened during the past week. Primarily, I learned two things: one is that they actually physically record their resuscitations. This includes the patient's EKG, ventilations, depth and frequency of chest compressions and even audio - audio! as in what the team is saying around the patient as they are coding them. That is so cool! The software gives you a full report, placing EKG reading, respiratory curves, chest compressions, end-tidal CO2 as well as information on whether or not the patient had a pulse at the time on time-synced visual graphs with the option of playing the audio at any time. That's so awesome for discussing what went right or wrong during the traditionally hectic conditions of a code situation which is exactly what they did. We have to have this in Germany.
And the other thing that I learned today was actually another piece of evidence that Americans are crazy. In a nice presentation on the benefit of post-code hypothermia the ED presenter mentioned this report, where investigators placed nine healthy volunteers (read: medstudents) under general anesthesia (yes, intubated and all!) to infuse them with ice water and see how their temperature drops. If you don't believe me, click on the link. Combine this with the concept of fecal transplants and you have definite proof beyond any reasonable doubt that these people are loco.
Allright, I'm going to let you go for now. I'll be done with the hospital exactly a week from today and flying back to Germany two days after that.
There are two things you should be able to expect from me during the upcoming days .. one should be a comprehensive review of the two months I've spent here and another should be a discussion on what the heck I want to do with my life (you definitely don't have to read the latter).
Blog to you later.
When I did work last week though I kept surprising myself by having a lot of answers during discussions and rounds. Especially with this one attending that "rounded" with us at his desk (much like the very first renal attending). He was a stud, appeared very young and overflowing with confidence, obviously was working out and judging from the pictures in his office he had his trophy wife tucked away (OK now I'm going a bit too far). Obviously, he was knowledgeable - you don't become an attending for nothing here. So while rounding in his office with Missy and the female intern on the team as soon as I started presenting my patient he'd say that we were going to have a "guy discussion" from now on, which apparently meant that we'd leave political correctness and etiquette aside - which was very refreshing and fun.
I didn't see much of that attending - he only filled in for the regular one that day. But from what I have experienced and heard about him I guess he is an extremely - maybe overly - confident guy that will be your best friend and not worry too much about taking care of patients himself as long as everything goes well. Apparently though, the yelling starts if ever things go south and he may ultimately be made responsible for something he should have taken more care of. So he's a nice, extremely suave and cool guy and he does seem to know his stuff but I still wouldn't want him as my attending - whether I'm on his team OR his patient.
But like I said, my experience with him was brief.
Over the weekend, like I said, I was sick and didn't do much except raiding the pharmacy for cold medication that turned out to be placebos for the most part - including the facial tissues. The stuff they sell there really is a very bad joke. Unless you use at least three of those tissues at once you might as well blow your nose into your hand directly. While at home with my headache I did get started typing down an exposé of the mentoring project the Chicago group has been working on. As of last night, it was up to 10 typed pages, I'm still waiting for the rest of the group to read it and sign off on it so we can pass the first drafts on to the good people in Boston and Munich. But I have high hopes for the next project meeting tonight at 6pm.
In other news, the service has been very light these past days and I was able to attend a lot of conferences today. Among them was a so-called "code review" where they discussed a few of the Dr. Cart (=cardiac arrest) calls that had happened during the past week. Primarily, I learned two things: one is that they actually physically record their resuscitations. This includes the patient's EKG, ventilations, depth and frequency of chest compressions and even audio - audio! as in what the team is saying around the patient as they are coding them. That is so cool! The software gives you a full report, placing EKG reading, respiratory curves, chest compressions, end-tidal CO2 as well as information on whether or not the patient had a pulse at the time on time-synced visual graphs with the option of playing the audio at any time. That's so awesome for discussing what went right or wrong during the traditionally hectic conditions of a code situation which is exactly what they did. We have to have this in Germany.
And the other thing that I learned today was actually another piece of evidence that Americans are crazy. In a nice presentation on the benefit of post-code hypothermia the ED presenter mentioned this report, where investigators placed nine healthy volunteers (read: medstudents) under general anesthesia (yes, intubated and all!) to infuse them with ice water and see how their temperature drops. If you don't believe me, click on the link. Combine this with the concept of fecal transplants and you have definite proof beyond any reasonable doubt that these people are loco.
Allright, I'm going to let you go for now. I'll be done with the hospital exactly a week from today and flying back to Germany two days after that.
There are two things you should be able to expect from me during the upcoming days .. one should be a comprehensive review of the two months I've spent here and another should be a discussion on what the heck I want to do with my life (you definitely don't have to read the latter).
Blog to you later.
Friday, May 18, 2007
Case report
The very first patient I had seen in this hospital - the one Jen sent me to see the morning of my very first day here - has just been presented to the residents in morning report. The 50.000 IU of vitamin D per day for months. The attending overseeing the presentation shook his head in the end and said this is something you will hardly ever see.
Except if you're a student fresh from Germany starting on renal consults.
Except if you're a student fresh from Germany starting on renal consults.
Wednesday, May 16, 2007
Over time.
I had a very good one and a half days.
They'd probably not be very good by everyone's standards as I've been in the hospital for 26 of the past 33 hours.
So here's how that happened. Yesterday started at 7:30 with critical care rounds again, I was pretty tired after around four hours of sleep - it had gotten rather hot and humid in Chicago that night and I needed to wait for Monday's episode of Heroes to download and be watched, obviously. But it went on to be a pretty normal day on the heart failure team. I was still enjoying having a load of time to go to all the conferences, with ample time to check on the three patients on our service. Jess was in clinic, but that didn't matter too much. It only meant that we'd be rounding a tiny bit later than we were used to, started maybe at around 3pm. A patient from the critical care unit was in surgery at that time and on our way to a lecture by a German liver surgeon we met his family. News from the OR had thus far been good, except for the fact that he was oozing blood just about everywhere, since he was on argatroban being heparin-intolerant which is non-reversible. So Brainy answered their questions and told them that they'd just have to wait for the bleeding to stop and that things would be fine. Even at that point in time, she was a little too definite with that last statement for my tastes when talking about a very sick patient from the unit undergoing open heart surgery.
Brainy and I went to the lecture, we were sitting rather isolatedly amidst all the surgeons. As it seemed, Brainy really didn't have any barriers when it comes to hierarchy and the likes. It was awesome. From the way we talked, joked around and exchanged candy in there she might as well have been a medstudent or I may have been an attending or we could basically just have been friends. I mean I really appreciate it and I'd love to see it the same way when or if it ever will be the other way around, with me not on the bottom end of the hierarchy I mean. Unfortunately, Brainy was paged during the lecture that the patient had died on the table, so she left and brought the bad news to the family.
Now, CS had told us two days before that she had changed to the cardiology inpatient service and was going to be on call yesterday. There were no U of C medstudents with her that night so she had invited any two of us to join her and admit cardiology patients that may come in. She was also planning on continuing the little EKG tutorial she had once started with us at six and had asked us to decide upon the two of us that would be on call with her yesterday. I figured, we might as well do that together during the tutorial since I expected all of us to be there. Unfortunately, I learned through a page during the lecture by the German guy that EKGs were cancelled. During the day, some of us had talked about who wanted to go on call and it seemed that not all were interested to do it and people from the second wave of the German invasion were kind enough to say that they'd probably have more opportunities to get a taste of on call inpatient admissions. Nevertheless, when I paged CS after the lecture at 6pm, I fully expected the jury still to be out on who'd be doing it.
"Philip, yes. Come down to the ER, Nema's already here and I have a patient for you."
So that was that then, it seemed.
Apparently though, my questionably bad luck with on call nights has turned since our service got slammed last night. CS was actively and actually sweating with the number of patients pouring in and that was the main reason why I was actually in the hospital until almost midnight - so six hours later. CS would not let me see more than one patient, but she wanted to hear my entire presentation on her and go through assessment and plan before she'd let me present to the attending the next morning. That was not an easy thing to get done while new patients required a cardiology bed left and right and CS was wheathering the storm. Still, she took a remarkable amount of time to listen to our presentations and give us hints and corrections for when we'd present to the attending the next day. So apparently the deal was that I should just see one patient and then go home - which is what I did. From what I heard from CS, their attending was going to arrive around 9 the next day and I was to present the patient I saw during their rounds which would be around then.
So I went home and slept. Critical care rounds this morning had unfortunately been pushed up to 7am, so I guess I wasn't really all that fresh again when I came to the hospital this morning. This time though, I arrived before Brainy (so far they had always been rounding for at least five minutes before I came stumbling through the door). So I paged my new fellow on the general cardiology consult team (because I was actually switching teams today, from heart failure to general cardiology). I had never seen her or heard of her in the hospital - I guess she must have been away, maybe on vacation before. I should ask her about that. When Brainy came, we rounded for just half an hour until we went up to cardiology case report conference at 7:30. The cases were pretty interesting. At 8:30, the conference was done. Walking out of the conference room, Brainy saw the intern that was going to be on cards consults with me and introduced us. While we were still walking down the halls, I got a page from CS at 8:36 reading "Phil, rounds in 5th fl WR now. Thx, CS".
Uhm, ok. So I went to the workroom where last night's team was assembled - CS, the two interns, Nema and myself. CS asked me whether I had checked up on my patient and was displeased to hear that I hadn't - I thought I still had time. One of the interns had grabbed the morning vitals and labs on the patient though and kindly brought me up to speed before the attending came. When he did, we went to a little windowless conference room (apparently nicknamed the "Bat Cave" by some as I had learned the night before), sat down and got introduced. The attending asked for our names and pager numbers. At first, I said he wasn't going to need my pager since I wasn't going to be on his service. Turns out I was wrong, though, since he would also be the attending for the general cardiology consult service.
Speaking of which, I hadn't heard back yet from the fellow of that service that I had paged at 7am. But hey, I tried to touch base .. what more could I do. So after that short introduction, the on call team started rounding with the attending and I just followed along, since I didn't have anything else to do anyway. While they were seeing the first patient, which was not mine, I paged my new fellow again and this time she did respond. I talked to her on the phone while the team was rounding, it was around 9:20. The new fellow, let's call her Missy, said she was just on her way in and that I didn't have to come in this early. I told her that I had just come for CCU rounds and the conference. She said "oh, OK" and then asked me to just hang out until she'd get there. I told her what I was doing, that I was rounding with the on-call team from last night because I had a patient to present. At that point she got confused and asked who I was again. I reiterated and explained the whole thing, emphasizing the fact that me staying at night was an exceptional thing but already then I feared she would expect me to know much more about what I was doing than I actually did. We saw another patient first, then Nema's and only then did we come up to mine, it was around 10:30 then. Now here's where the main part about the goodness started - I think the presentation went very well. It didn't seem like I had forgotten anything major and sometimes must even have sounded like I knew what I was saying. Having just come off the heart failure team, I was even able to back up some of what I said in the discussion of the plan for the patient with actual trial data. Of course the attending knew much more about the subject and taught us some new stuff but I still think it went exceptionally well. Unfortunately, now I seemed to have two people to convince not to expect too much from me since I seemed to have made rather favorable first impressions on both the fellow and the attending. They're going to be so much more disappointed when they find out the truth about me after initially having this distorted picture of me being highly competent. I would have been much more comfortable if they took me for the rookie I am.
Unfortunately, when I met my current team, fellow and intern a little bit later, Missy handed me an EKG strip to interpret. Despite the fact that I strongly emphasized how little I knew (which as feared, Missy didn't believe) I interpreted the strip correctly as being sinus with incomplete left bundle branch block that turned into overdrive-suppression by a ventricular automaticity focus that paced the heart only slightly above the sinus rate. At that point, Missy completely stopped listening to me when I pleaded that I didn't know what I was doing. So now I was screwed.
She gave me one of the new patients she got today to see and while I was presenting this patient to the attending, I got a glimpse of what was to come when they finally realize the extent of my knowledge. Missy asked me what I thought of the use of "Cardizem" in this case. I truthfully replied that I didn't even know what that drug was. At that moment, I caught a short glimpse of astonished jaw-dropping on Missy's side. I asked her whether that was a brand name and she apologized with a hint of relief that it was diltiazem. After that, I could answer her question somewhat satisfyingly but I'm not sure I want to see what happens when they find out how vague my understanding of things like the anatomy of coronary arteries or cardiology in general actually is.
Still, today was a good day and I can now comfortably watch the new episodes of 24, House and Gilmore Girls, since I don't have to be back in that place until 9am.
Yay!
Blog to you later.
They'd probably not be very good by everyone's standards as I've been in the hospital for 26 of the past 33 hours.
So here's how that happened. Yesterday started at 7:30 with critical care rounds again, I was pretty tired after around four hours of sleep - it had gotten rather hot and humid in Chicago that night and I needed to wait for Monday's episode of Heroes to download and be watched, obviously. But it went on to be a pretty normal day on the heart failure team. I was still enjoying having a load of time to go to all the conferences, with ample time to check on the three patients on our service. Jess was in clinic, but that didn't matter too much. It only meant that we'd be rounding a tiny bit later than we were used to, started maybe at around 3pm. A patient from the critical care unit was in surgery at that time and on our way to a lecture by a German liver surgeon we met his family. News from the OR had thus far been good, except for the fact that he was oozing blood just about everywhere, since he was on argatroban being heparin-intolerant which is non-reversible. So Brainy answered their questions and told them that they'd just have to wait for the bleeding to stop and that things would be fine. Even at that point in time, she was a little too definite with that last statement for my tastes when talking about a very sick patient from the unit undergoing open heart surgery.
Brainy and I went to the lecture, we were sitting rather isolatedly amidst all the surgeons. As it seemed, Brainy really didn't have any barriers when it comes to hierarchy and the likes. It was awesome. From the way we talked, joked around and exchanged candy in there she might as well have been a medstudent or I may have been an attending or we could basically just have been friends. I mean I really appreciate it and I'd love to see it the same way when or if it ever will be the other way around, with me not on the bottom end of the hierarchy I mean. Unfortunately, Brainy was paged during the lecture that the patient had died on the table, so she left and brought the bad news to the family.
Now, CS had told us two days before that she had changed to the cardiology inpatient service and was going to be on call yesterday. There were no U of C medstudents with her that night so she had invited any two of us to join her and admit cardiology patients that may come in. She was also planning on continuing the little EKG tutorial she had once started with us at six and had asked us to decide upon the two of us that would be on call with her yesterday. I figured, we might as well do that together during the tutorial since I expected all of us to be there. Unfortunately, I learned through a page during the lecture by the German guy that EKGs were cancelled. During the day, some of us had talked about who wanted to go on call and it seemed that not all were interested to do it and people from the second wave of the German invasion were kind enough to say that they'd probably have more opportunities to get a taste of on call inpatient admissions. Nevertheless, when I paged CS after the lecture at 6pm, I fully expected the jury still to be out on who'd be doing it.
"Philip, yes. Come down to the ER, Nema's already here and I have a patient for you."
So that was that then, it seemed.
Apparently though, my questionably bad luck with on call nights has turned since our service got slammed last night. CS was actively and actually sweating with the number of patients pouring in and that was the main reason why I was actually in the hospital until almost midnight - so six hours later. CS would not let me see more than one patient, but she wanted to hear my entire presentation on her and go through assessment and plan before she'd let me present to the attending the next morning. That was not an easy thing to get done while new patients required a cardiology bed left and right and CS was wheathering the storm. Still, she took a remarkable amount of time to listen to our presentations and give us hints and corrections for when we'd present to the attending the next day. So apparently the deal was that I should just see one patient and then go home - which is what I did. From what I heard from CS, their attending was going to arrive around 9 the next day and I was to present the patient I saw during their rounds which would be around then.
So I went home and slept. Critical care rounds this morning had unfortunately been pushed up to 7am, so I guess I wasn't really all that fresh again when I came to the hospital this morning. This time though, I arrived before Brainy (so far they had always been rounding for at least five minutes before I came stumbling through the door). So I paged my new fellow on the general cardiology consult team (because I was actually switching teams today, from heart failure to general cardiology). I had never seen her or heard of her in the hospital - I guess she must have been away, maybe on vacation before. I should ask her about that. When Brainy came, we rounded for just half an hour until we went up to cardiology case report conference at 7:30. The cases were pretty interesting. At 8:30, the conference was done. Walking out of the conference room, Brainy saw the intern that was going to be on cards consults with me and introduced us. While we were still walking down the halls, I got a page from CS at 8:36 reading "Phil, rounds in 5th fl WR now. Thx, CS".
Uhm, ok. So I went to the workroom where last night's team was assembled - CS, the two interns, Nema and myself. CS asked me whether I had checked up on my patient and was displeased to hear that I hadn't - I thought I still had time. One of the interns had grabbed the morning vitals and labs on the patient though and kindly brought me up to speed before the attending came. When he did, we went to a little windowless conference room (apparently nicknamed the "Bat Cave" by some as I had learned the night before), sat down and got introduced. The attending asked for our names and pager numbers. At first, I said he wasn't going to need my pager since I wasn't going to be on his service. Turns out I was wrong, though, since he would also be the attending for the general cardiology consult service.
Speaking of which, I hadn't heard back yet from the fellow of that service that I had paged at 7am. But hey, I tried to touch base .. what more could I do. So after that short introduction, the on call team started rounding with the attending and I just followed along, since I didn't have anything else to do anyway. While they were seeing the first patient, which was not mine, I paged my new fellow again and this time she did respond. I talked to her on the phone while the team was rounding, it was around 9:20. The new fellow, let's call her Missy, said she was just on her way in and that I didn't have to come in this early. I told her that I had just come for CCU rounds and the conference. She said "oh, OK" and then asked me to just hang out until she'd get there. I told her what I was doing, that I was rounding with the on-call team from last night because I had a patient to present. At that point she got confused and asked who I was again. I reiterated and explained the whole thing, emphasizing the fact that me staying at night was an exceptional thing but already then I feared she would expect me to know much more about what I was doing than I actually did. We saw another patient first, then Nema's and only then did we come up to mine, it was around 10:30 then. Now here's where the main part about the goodness started - I think the presentation went very well. It didn't seem like I had forgotten anything major and sometimes must even have sounded like I knew what I was saying. Having just come off the heart failure team, I was even able to back up some of what I said in the discussion of the plan for the patient with actual trial data. Of course the attending knew much more about the subject and taught us some new stuff but I still think it went exceptionally well. Unfortunately, now I seemed to have two people to convince not to expect too much from me since I seemed to have made rather favorable first impressions on both the fellow and the attending. They're going to be so much more disappointed when they find out the truth about me after initially having this distorted picture of me being highly competent. I would have been much more comfortable if they took me for the rookie I am.
Unfortunately, when I met my current team, fellow and intern a little bit later, Missy handed me an EKG strip to interpret. Despite the fact that I strongly emphasized how little I knew (which as feared, Missy didn't believe) I interpreted the strip correctly as being sinus with incomplete left bundle branch block that turned into overdrive-suppression by a ventricular automaticity focus that paced the heart only slightly above the sinus rate. At that point, Missy completely stopped listening to me when I pleaded that I didn't know what I was doing. So now I was screwed.
She gave me one of the new patients she got today to see and while I was presenting this patient to the attending, I got a glimpse of what was to come when they finally realize the extent of my knowledge. Missy asked me what I thought of the use of "Cardizem" in this case. I truthfully replied that I didn't even know what that drug was. At that moment, I caught a short glimpse of astonished jaw-dropping on Missy's side. I asked her whether that was a brand name and she apologized with a hint of relief that it was diltiazem. After that, I could answer her question somewhat satisfyingly but I'm not sure I want to see what happens when they find out how vague my understanding of things like the anatomy of coronary arteries or cardiology in general actually is.
Still, today was a good day and I can now comfortably watch the new episodes of 24, House and Gilmore Girls, since I don't have to be back in that place until 9am.
Yay!
Blog to you later.
Tuesday, May 15, 2007
Americans.
Morning report today focused on long-term care of patients with chronic conditions like diabetes or hypertension and the difficulties we are faced with in that area. So the first case was on a 64-year-old african american female who was - of course - overweight. We were told the story of how she started out on one medication in 2003 and when her blood pressures never responded in subsequent clinic visits, how her regimen was gradually extended to four different blood pressure medications.
At this point in the slide show, the next slide posed the question "what else can you think of to optimize treatment of this patient's hypertension?" to the audience. I was convinced that I knew what this slide was going to show. To my surprise, what they were looking for here were the questions "is the patient taking her medications?" - all right, good one. "Can the patient afford her medications?" - uhm, I see. "Does the patient have access to her medications?" - as in - can she get her obese self to the pharmacy and back? I guess that's a valid question too. But that was it.
Whatever happened to "Did anyone ever talk to this patient about less McDonalds and more exercise?" Is educating people about sodium intake and physical exercise and the likes of that so out of fashion that it doesn't even come up in a discussion of the management of primary hypertension?
At this point in the slide show, the next slide posed the question "what else can you think of to optimize treatment of this patient's hypertension?" to the audience. I was convinced that I knew what this slide was going to show. To my surprise, what they were looking for here were the questions "is the patient taking her medications?" - all right, good one. "Can the patient afford her medications?" - uhm, I see. "Does the patient have access to her medications?" - as in - can she get her obese self to the pharmacy and back? I guess that's a valid question too. But that was it.
Whatever happened to "Did anyone ever talk to this patient about less McDonalds and more exercise?" Is educating people about sodium intake and physical exercise and the likes of that so out of fashion that it doesn't even come up in a discussion of the management of primary hypertension?
Monday, May 14, 2007
Sociology
Hey reader,
today was another good day.
It started off with me coming to critical care unit rounds at 7:30am that my attending had invited me to last week. When I met them, they informed me though that there'd be a conference on pulmonary hypertension upstairs. Oh and there would be bagels a resident said. Sold!
The conference was interesting. I met Jess there. She told me she'd be doing a lot of right heart caths today so I stopped by there after the conference. There, she just asked me to check up on our old patients - the whole service! Now that would be much more of a shocker if the service had consisted of more than three patients. Muahahah!
This way I had leisure to check out morning report at 10, which was a somewhat-interesting discussion on how the U of C hospitals should extend community clinic services. Between around 11:15 and noon I actually did look up the labs on the patients and checked in on them. I was back in A700 in time for the lunch conference :D .
For the first time (in the history of the residency program as I later learned), there was actually a drug rep there who sponsored the lunch and handed out journal articles and leaflets. I conveniently (but honestly) missed the piece of paper on the wall stating that this lunch was restricted to interns and sub-interns. I guess that's why the rep did not hand out the articles to me. I'm clearly identifiable by my horrible short coat. A second-wave medstudent from Germany whom we had warned was wearing his regular long coat, so he was "welcome" to the lunch I guess.
Well, whatever. I got food.
After I sat down, somehow a conversation with the person next to me began. Turned out that he, as well, wasn't really entitled to his long, white coat. He turned out to be a sociology major, there to observe. His thesis had something to do with social networks in the medical profession and specifically how people are perceived by others, like some people that are deemed knowledgeable by their peers yet not arrogant, but pleasant to work with. Like my current attending. He had been following a lot of medical teams around over almost a year by now and only had time to come to the lunch meeting for the first time today. He, of course, was very interested in what I had to say about my impressions here and I very much enjoyed exchanging them with someone who was in very similar shoes. We both had been thrown into these "teams" that were alien in many ways for either of us. The noon conference on an interesting case of lupus complicated by myocarditis interrupted us, but on the whole we spent about 2 hours talking. And I did have the time to do that. That was so nice.
And with Brainy (who will be a prime subject for his research) and the mentoring program we're trying to build in Germany and differences between US and German systems we did not run out of discussion topics, so we said we'd meet for lunch again some time.
So around 2:30pm I strolled back to the cath lab, where Jess was doing the same thing I had left her with: right heart caths, just got done doing the seventh. While she was almost done, she asked me to page Brainy to find out when she would want to round. Turned out she was right through the doors of the cath lab in the cardiac critical care unit (nice infrastructure!) basically waiting to round with us. I actually brought her into the cath lab, because the first patient we'd be rounding on had just had pieces of his replacement heart removed by Jess.
So we saved ourselves that trip. Mentioning that second patient only evoked tirades from the female rest of the team about what a sexist womanizing jerk he was. Seeking to provoke, as I usually do, I threw in that I liked him. My attending then explained to me that the advantage of her being smaller than me was that she was perfectly positioned for a right hook to my jaw. She demonstrated the movement and I saw her point. Dude, can you imagine a German attending kidding around with a mere medstudent like that?
They ended up deciding that we didn't need to see that patient that day.
That left only one patient to see, which we did. He had been sent to the floor from the ICU today and was ostensibly doing just peachy.
The three of us subsequently chatted pleasantly for a while until Brainy sent us home around 4.
Brilliant!
today was another good day.
It started off with me coming to critical care unit rounds at 7:30am that my attending had invited me to last week. When I met them, they informed me though that there'd be a conference on pulmonary hypertension upstairs. Oh and there would be bagels a resident said. Sold!
The conference was interesting. I met Jess there. She told me she'd be doing a lot of right heart caths today so I stopped by there after the conference. There, she just asked me to check up on our old patients - the whole service! Now that would be much more of a shocker if the service had consisted of more than three patients. Muahahah!
This way I had leisure to check out morning report at 10, which was a somewhat-interesting discussion on how the U of C hospitals should extend community clinic services. Between around 11:15 and noon I actually did look up the labs on the patients and checked in on them. I was back in A700 in time for the lunch conference :D .
For the first time (in the history of the residency program as I later learned), there was actually a drug rep there who sponsored the lunch and handed out journal articles and leaflets. I conveniently (but honestly) missed the piece of paper on the wall stating that this lunch was restricted to interns and sub-interns. I guess that's why the rep did not hand out the articles to me. I'm clearly identifiable by my horrible short coat. A second-wave medstudent from Germany whom we had warned was wearing his regular long coat, so he was "welcome" to the lunch I guess.
Well, whatever. I got food.
After I sat down, somehow a conversation with the person next to me began. Turned out that he, as well, wasn't really entitled to his long, white coat. He turned out to be a sociology major, there to observe. His thesis had something to do with social networks in the medical profession and specifically how people are perceived by others, like some people that are deemed knowledgeable by their peers yet not arrogant, but pleasant to work with. Like my current attending. He had been following a lot of medical teams around over almost a year by now and only had time to come to the lunch meeting for the first time today. He, of course, was very interested in what I had to say about my impressions here and I very much enjoyed exchanging them with someone who was in very similar shoes. We both had been thrown into these "teams" that were alien in many ways for either of us. The noon conference on an interesting case of lupus complicated by myocarditis interrupted us, but on the whole we spent about 2 hours talking. And I did have the time to do that. That was so nice.
And with Brainy (who will be a prime subject for his research) and the mentoring program we're trying to build in Germany and differences between US and German systems we did not run out of discussion topics, so we said we'd meet for lunch again some time.
So around 2:30pm I strolled back to the cath lab, where Jess was doing the same thing I had left her with: right heart caths, just got done doing the seventh. While she was almost done, she asked me to page Brainy to find out when she would want to round. Turned out she was right through the doors of the cath lab in the cardiac critical care unit (nice infrastructure!) basically waiting to round with us. I actually brought her into the cath lab, because the first patient we'd be rounding on had just had pieces of his replacement heart removed by Jess.
So we saved ourselves that trip. Mentioning that second patient only evoked tirades from the female rest of the team about what a sexist womanizing jerk he was. Seeking to provoke, as I usually do, I threw in that I liked him. My attending then explained to me that the advantage of her being smaller than me was that she was perfectly positioned for a right hook to my jaw. She demonstrated the movement and I saw her point. Dude, can you imagine a German attending kidding around with a mere medstudent like that?
They ended up deciding that we didn't need to see that patient that day.
That left only one patient to see, which we did. He had been sent to the floor from the ICU today and was ostensibly doing just peachy.
The three of us subsequently chatted pleasantly for a while until Brainy sent us home around 4.
Brilliant!
Sunday, May 13, 2007
Catching up
Hello readers,
I grew a bit tired of blogging, which is strange since I have basically way fewer patients to see and therefore more time during the day.
On Wednesday, yet again, my attending changed. And if I was impressed with the last one, this new one is even more incredible. She has never admitted to her actual age, keeps making up numbers jokingly. So I'll have to guess her at around 35. She's born in Chicago, daughter of a sociology major and a physician somewhere in Switzerland, I think. She studied European history in college, which is where her comments about Hegel she shot at me during rounds must have come from.
When I first saw her, in the ER, she was in the middle of listening to the presentation of a patient by the ER resident. She was scribbling down things on a pad, looking up the patient's labs and sending text pages on the computer while intermittently grabbing the phone when her pages were answered. In between, the attending shot short questions towards the resident when she had forgotten to mention something. She would talk fast, but friendly. It seemed like she could remind you that the thing between left atrium and ventricle was the mitral valve and still make you believe that it wasn't a big thing to forget and that it could happen to anyone. In the middle of all of this, one of her ever-moving hands reached out towards me, she smiled and introduced herself to me with her nickname and last name. I had time to shake that hand and say my own first name (I have given up using my last name permanently over here) before the fraction of her focus I was allotted at that time was taken away again. I didn't mind, on the contrary, I was pleased with her productivity. Rounds would be good.
And I thought Jen was the embodiment of the ability to multitask - this new attending was like Jen with a quad core processor.
A resident I know from renal consults, who is now on the ICU team that the new attending also rounds with, found a nice way to describe what her impact on her surroundings is. While the new attending - let's call her Brainy (heheh) - was busy working up a patient with the rest of the team and the ICU staff, the resident and I stood to the side and he muttered to me
"dude .. she's like a tornado."
True. But now in this picture that I've drawn so far, you'd probably imagine Brainy to be excited or appear stressed-out. And here's the strange thing, that couldn't be further from the truth. She's more laid back than almost any attending (except for the first one I had over here, no one can match that guy when it comes to taking life easy). She'll never speak in anything but a calm tone albeit fast and direct. Every other phrase coming out of her mouth will be ironic or funny in some other way but to the point. At the same time, she will never try to make you feel inferior (you just inherently do) despite the fact that the collective jaws of the heart failure team will drop every so often when she just never seems to run out of answers to just about any question there is.
For example - a patient post heart transplant turned up with undulating fevers that no one in the hospital could find a reason for in the past weeks. Outside the patient's room, while flying through the pages of the chart, Brainy asked for the patient's tacrolimus level (an immunosuppressant for the transplant). It was rather high. Brainy frowned a bit, skipped ahead to the medications list and then asked the nurse practitioner to hold his tacrolimus dose for three days. She also said that they shouldn't even bother drawing blood for another level tonight, it would be high again. Naturally, the team sported blank expressions and one of us managed to blurt out the question how she came to these conclusions. She pointed at the medication list, specifically a rather new order of voriconazole and looked at us with wide, but friendly eyes. This didn't help us much so she quickly explained that voriconazole will inhibit cytochrome P450 3A4/5, which is responsible for tacrolimus metabolism. Uh-huh. Well - you can still write this off to being her tools of the trade. She's in heart failure and involved with a lot of transplants. Big deal. But it got better.
After asking this same patient questions that we could halfway relate to about contact to kettle, cats and rabbits the patient said he hadn't had any contact to those kinds of animals. Oh, just his niece had brought a turtle. Instantly, Brainy asked the nurse practitioner to add cultures for salmonella. Turtles have salmonella? Of course they do. Did any of the rest of the team know that? Nope. After Brainy imparted some more wisdom on the patient (including how to clean your ears without a q-tip) we left that patient's room and Jess confronted Brainy with "how do you know all this?". Brainy just downplayed it as not being a big deal as she would always do.
But this woman is not limited to theoretical knowledge. We rounded on another patient who had broken his leg while carrying another person's heart in his chest (which is where we came in). He was going to be operated on by ortho as soon as the swelling in his leg would go down and his platelets (that were down for some unknown reason) were back up. Now, cooling the leg would have been helpful with the swelling, right? So Brainy asked the primary team's resident that took care of the patient why there was no ice on the patient's broken leg. The resident replied that he had written for it, but the nurses couldn't do it because the ice packs they had were too small for the leg, they'd always fall off. Brainy abruptly went to the nearest garbage container, took out the trash bag and gave it to me to hold, grabbed a fresh garbage bag that they keep inside these containers, went to the ice machine in the nourishment room, filled it and that was that. While doing all this, however, she would NOT give anyone a hard time about it. She would not even say anything about people having lost common sense and practical skills somewhere around their medical training. I challenge anyone to not even making a single remark in that direction in this situation.
The next day, that same patient was to receive one of those little plastic machines that you blow into for breathing exercise. You know, with the three little balls you have to blow up. The resident said he agreed that he should have received that thing and started practicing the sooner the better but the nurses just hadn't gotten around to giving him one yet despite him writing the order. He was a rather tall resident, so he had to duck when Brainy opened a closet high up on the wall right in front of the patient's door. It contains a number of frequently-used items in patient care, such as urine cups, syringes, foley bags - and the little plastic breathing exercisers. She took one and handed it to the resident. She also advised the patient to drink a lot of cherry juice and stay away from watermelons during the summer. By now, I have totally forgotten why but I'm sure it makes total sense just like all the other pieces of knowledge this attending has been spraying out.
Can you tell I'm a fan?
Now don't get me wrong, I believe I couldn't stand her personally if she kept up the pace she brings to work every day. But since I only see her at work and we have a minuscule patient load I get to profit immensely from her - since she enjoys teaching.
Problem is that CS, Jess and Brainy all keep stacking journal articles on me "to read" - the number of these being only directly proportional to the amount of bad conscience I come to work with, since the number of articles I'll read will remain constant right around zero.
In other news, after interviewing the director and an associate director of the residency program in internal medicine the chicagoans got together and worked on the mentoring system we're supposed to institute at our medschool back in Munich. It's slowly taking shape and at least I for one believe that it's going to be an extremely cool program.
and worked on the mentoring system we're supposed to institute at our medschool back in Munich. It's slowly taking shape and at least I for one believe that it's going to be an extremely cool program.
And on Friday all of the chicagoans came to Looptopia - a brand new festival premiering this year in Chicago celebrating the loop. There were artists on the streets and numerous events all over the buildings around the loop. It wasn't that much of a success for us though, since we didn't have much of a plan of what events to go to and we ended up waiting in line most of the time and giving up and walking out somewhere halfway through.
There were artists on the streets and numerous events all over the buildings around the loop. It wasn't that much of a success for us though, since we didn't have much of a plan of what events to go to and we ended up waiting in line most of the time and giving up and walking out somewhere halfway through.
Allright, that should do for now and keep you busy. I'm off to do happier things like finally finishing that book on EKGs or something.
Blog to you later.
I grew a bit tired of blogging, which is strange since I have basically way fewer patients to see and therefore more time during the day.
On Wednesday, yet again, my attending changed. And if I was impressed with the last one, this new one is even more incredible. She has never admitted to her actual age, keeps making up numbers jokingly. So I'll have to guess her at around 35. She's born in Chicago, daughter of a sociology major and a physician somewhere in Switzerland, I think. She studied European history in college, which is where her comments about Hegel she shot at me during rounds must have come from.
When I first saw her, in the ER, she was in the middle of listening to the presentation of a patient by the ER resident. She was scribbling down things on a pad, looking up the patient's labs and sending text pages on the computer while intermittently grabbing the phone when her pages were answered. In between, the attending shot short questions towards the resident when she had forgotten to mention something. She would talk fast, but friendly. It seemed like she could remind you that the thing between left atrium and ventricle was the mitral valve and still make you believe that it wasn't a big thing to forget and that it could happen to anyone. In the middle of all of this, one of her ever-moving hands reached out towards me, she smiled and introduced herself to me with her nickname and last name. I had time to shake that hand and say my own first name (I have given up using my last name permanently over here) before the fraction of her focus I was allotted at that time was taken away again. I didn't mind, on the contrary, I was pleased with her productivity. Rounds would be good.
And I thought Jen was the embodiment of the ability to multitask - this new attending was like Jen with a quad core processor.
A resident I know from renal consults, who is now on the ICU team that the new attending also rounds with, found a nice way to describe what her impact on her surroundings is. While the new attending - let's call her Brainy (heheh) - was busy working up a patient with the rest of the team and the ICU staff, the resident and I stood to the side and he muttered to me
"dude .. she's like a tornado."
True. But now in this picture that I've drawn so far, you'd probably imagine Brainy to be excited or appear stressed-out. And here's the strange thing, that couldn't be further from the truth. She's more laid back than almost any attending (except for the first one I had over here, no one can match that guy when it comes to taking life easy). She'll never speak in anything but a calm tone albeit fast and direct. Every other phrase coming out of her mouth will be ironic or funny in some other way but to the point. At the same time, she will never try to make you feel inferior (you just inherently do) despite the fact that the collective jaws of the heart failure team will drop every so often when she just never seems to run out of answers to just about any question there is.
For example - a patient post heart transplant turned up with undulating fevers that no one in the hospital could find a reason for in the past weeks. Outside the patient's room, while flying through the pages of the chart, Brainy asked for the patient's tacrolimus level (an immunosuppressant for the transplant). It was rather high. Brainy frowned a bit, skipped ahead to the medications list and then asked the nurse practitioner to hold his tacrolimus dose for three days. She also said that they shouldn't even bother drawing blood for another level tonight, it would be high again. Naturally, the team sported blank expressions and one of us managed to blurt out the question how she came to these conclusions. She pointed at the medication list, specifically a rather new order of voriconazole and looked at us with wide, but friendly eyes. This didn't help us much so she quickly explained that voriconazole will inhibit cytochrome P450 3A4/5, which is responsible for tacrolimus metabolism. Uh-huh. Well - you can still write this off to being her tools of the trade. She's in heart failure and involved with a lot of transplants. Big deal. But it got better.
After asking this same patient questions that we could halfway relate to about contact to kettle, cats and rabbits the patient said he hadn't had any contact to those kinds of animals. Oh, just his niece had brought a turtle. Instantly, Brainy asked the nurse practitioner to add cultures for salmonella. Turtles have salmonella? Of course they do. Did any of the rest of the team know that? Nope. After Brainy imparted some more wisdom on the patient (including how to clean your ears without a q-tip) we left that patient's room and Jess confronted Brainy with "how do you know all this?". Brainy just downplayed it as not being a big deal as she would always do.
But this woman is not limited to theoretical knowledge. We rounded on another patient who had broken his leg while carrying another person's heart in his chest (which is where we came in). He was going to be operated on by ortho as soon as the swelling in his leg would go down and his platelets (that were down for some unknown reason) were back up. Now, cooling the leg would have been helpful with the swelling, right? So Brainy asked the primary team's resident that took care of the patient why there was no ice on the patient's broken leg. The resident replied that he had written for it, but the nurses couldn't do it because the ice packs they had were too small for the leg, they'd always fall off. Brainy abruptly went to the nearest garbage container, took out the trash bag and gave it to me to hold, grabbed a fresh garbage bag that they keep inside these containers, went to the ice machine in the nourishment room, filled it and that was that. While doing all this, however, she would NOT give anyone a hard time about it. She would not even say anything about people having lost common sense and practical skills somewhere around their medical training. I challenge anyone to not even making a single remark in that direction in this situation.
The next day, that same patient was to receive one of those little plastic machines that you blow into for breathing exercise. You know, with the three little balls you have to blow up. The resident said he agreed that he should have received that thing and started practicing the sooner the better but the nurses just hadn't gotten around to giving him one yet despite him writing the order. He was a rather tall resident, so he had to duck when Brainy opened a closet high up on the wall right in front of the patient's door. It contains a number of frequently-used items in patient care, such as urine cups, syringes, foley bags - and the little plastic breathing exercisers. She took one and handed it to the resident. She also advised the patient to drink a lot of cherry juice and stay away from watermelons during the summer. By now, I have totally forgotten why but I'm sure it makes total sense just like all the other pieces of knowledge this attending has been spraying out.
Can you tell I'm a fan?
Now don't get me wrong, I believe I couldn't stand her personally if she kept up the pace she brings to work every day. But since I only see her at work and we have a minuscule patient load I get to profit immensely from her - since she enjoys teaching.
Problem is that CS, Jess and Brainy all keep stacking journal articles on me "to read" - the number of these being only directly proportional to the amount of bad conscience I come to work with, since the number of articles I'll read will remain constant right around zero.
In other news, after interviewing the director and an associate director of the residency program in internal medicine the chicagoans got together
 and worked on the mentoring system we're supposed to institute at our medschool back in Munich. It's slowly taking shape and at least I for one believe that it's going to be an extremely cool program.
and worked on the mentoring system we're supposed to institute at our medschool back in Munich. It's slowly taking shape and at least I for one believe that it's going to be an extremely cool program.And on Friday all of the chicagoans came to Looptopia - a brand new festival premiering this year in Chicago celebrating the loop.
 There were artists on the streets and numerous events all over the buildings around the loop. It wasn't that much of a success for us though, since we didn't have much of a plan of what events to go to and we ended up waiting in line most of the time and giving up and walking out somewhere halfway through.
There were artists on the streets and numerous events all over the buildings around the loop. It wasn't that much of a success for us though, since we didn't have much of a plan of what events to go to and we ended up waiting in line most of the time and giving up and walking out somewhere halfway through.Allright, that should do for now and keep you busy. I'm off to do happier things like finally finishing that book on EKGs or something.
Blog to you later.
Monday, May 7, 2007
Finally!
Better late than never .. after playing basketball for a few hours with a couple of sociology students, we went for dinner and a few drinks in chinatown. Finally reminded me a bit of high school over here, when we used to take someone's car and go out to eat somewhere at least every other night.
Good times.
Of course, I still have not read those papers my fellow has given me that I should have been long done with. But since today was another "weird" day and we never "had a chance" to "sit down" and "discuss" as she put it and tomorrow is shaping up to be another one of those weird (or rather, usual) days I think I'll be just fine :)
Anyway, I need to catch up on missed sleep again after having been listening to a-capella-trash-metal till 2am last night (do ask!) and I need to have my liver work on the Tsingtao in my system.
Blog to you later.
Good times.
Of course, I still have not read those papers my fellow has given me that I should have been long done with. But since today was another "weird" day and we never "had a chance" to "sit down" and "discuss" as she put it and tomorrow is shaping up to be another one of those weird (or rather, usual) days I think I'll be just fine :)
Anyway, I need to catch up on missed sleep again after having been listening to a-capella-trash-metal till 2am last night (do ask!) and I need to have my liver work on the Tsingtao in my system.
Blog to you later.
Saturday, May 5, 2007
Small, strange world.
I've been getting used to weird coincidences lately. Still, today was a bit stranger than most other days.
The line at Hyde Park Produce was exceptionally long today, from the cash register all the way back to the deli counter. In line in front of me was a couple and the girl was wearing a sweater with a little label from the show "popstars". I couldn't refrain from asking whether you would actually have to be in the show to get a sweater like that or whether you could buy them. She turned bright red and kept saying how "peinlich" wearing the sweater was for her. Heheh. Anyway, she had a PhD in neuroscience and he was a post-doc in biochemistry, both from Germany naturally, with him currently working on tumor immunology with the same mouse strain I am (or used to be). He's using retroviral treatments though in contrast to my immunostimulatory molecules. There had to be a tiny difference, otherwise chances are I would have known him.
Anyway, that was the "small" part of the world - here's the strange part.
I went to the pharmacy afterwards to get water and milk, but also because I had a herpes blister on my lips (guess I may have been immunosuppressing myself lately with poor nutrition, little sleep and endogenous steroids). I quickly scanned the aisles of this huge (compared to German ones) pharmacy and then went to the "pharmacist"'s counter. Said pharmacist was apparently working in the aisles, the aids said. So they asked me whether they could help me. Sure enough, I thought, this is easy enough.
So I said
"I'm looking for some topical acyclovir for lip herpes."
- "What?"
"Acyclovir. Like in an ointment."
- "Uhhh .. do you have a prescription?"
"A prescription? No I don't. I have a herpes blister on my lip. Here. Look."
- "Uhhh .."
"I'm just looking for some acyclovir ointment to put on there."
- "Oh, you mean like a cold sore?"
"A what now?"
- "A cold sore."
"If that's what you call it."
- "Uhhh .. I think you're looking for Abreva."
"Am I. So where's that."
- "It should be there!" (Points to end of an aisle)
So I go look, there's several kinds of chap stick and finally I find a label of "Abreva" saying I should contact customer service for this. The pharmacist aids said if it wasn't there I should go up to the cash register.
So I got my milk and my two gallons of water and stepped up to the cash register, asking for Abreva. That prompted the person at the register to point to another rack of worthless chap stick among all the candy, lighters and magazines and to comment "we may be out of it".
I couldn't refrain from replying "Isn't this supposed to be a pharmacy?".
This building could house at least three full-fledged German pharmacies that carry multiple formulations of topical acyclovir which is one of the safest drugs in the world. And this 24h-open so-called pharmacy offers beans in a can, fresh milk and frozen pizza for crying out loud but nothing to take care of a friggin' blister on your lips.
That's messed up dude.
The line at Hyde Park Produce was exceptionally long today, from the cash register all the way back to the deli counter. In line in front of me was a couple and the girl was wearing a sweater with a little label from the show "popstars". I couldn't refrain from asking whether you would actually have to be in the show to get a sweater like that or whether you could buy them. She turned bright red and kept saying how "peinlich" wearing the sweater was for her. Heheh. Anyway, she had a PhD in neuroscience and he was a post-doc in biochemistry, both from Germany naturally, with him currently working on tumor immunology with the same mouse strain I am (or used to be). He's using retroviral treatments though in contrast to my immunostimulatory molecules. There had to be a tiny difference, otherwise chances are I would have known him.
Anyway, that was the "small" part of the world - here's the strange part.
I went to the pharmacy afterwards to get water and milk, but also because I had a herpes blister on my lips (guess I may have been immunosuppressing myself lately with poor nutrition, little sleep and endogenous steroids). I quickly scanned the aisles of this huge (compared to German ones) pharmacy and then went to the "pharmacist"'s counter. Said pharmacist was apparently working in the aisles, the aids said. So they asked me whether they could help me. Sure enough, I thought, this is easy enough.
So I said
"I'm looking for some topical acyclovir for lip herpes."
- "What?"
"Acyclovir. Like in an ointment."
- "Uhhh .. do you have a prescription?"
"A prescription? No I don't. I have a herpes blister on my lip. Here. Look."
- "Uhhh .."
"I'm just looking for some acyclovir ointment to put on there."
- "Oh, you mean like a cold sore?"
"A what now?"
- "A cold sore."
"If that's what you call it."
- "Uhhh .. I think you're looking for Abreva."
"Am I. So where's that."
- "It should be there!" (Points to end of an aisle)
So I go look, there's several kinds of chap stick and finally I find a label of "Abreva" saying I should contact customer service for this. The pharmacist aids said if it wasn't there I should go up to the cash register.
So I got my milk and my two gallons of water and stepped up to the cash register, asking for Abreva. That prompted the person at the register to point to another rack of worthless chap stick among all the candy, lighters and magazines and to comment "we may be out of it".
I couldn't refrain from replying "Isn't this supposed to be a pharmacy?".
This building could house at least three full-fledged German pharmacies that carry multiple formulations of topical acyclovir which is one of the safest drugs in the world. And this 24h-open so-called pharmacy offers beans in a can, fresh milk and frozen pizza for crying out loud but nothing to take care of a friggin' blister on your lips.
That's messed up dude.
Friday, May 4, 2007
Murphy's Law or just bad karma?
Miraculously, my team was willing to let me go at 4pm today. 4pm!
But hey, that doesn't sound like something that could happen to me, does it? Of course not. CS had scheduled a meeting for us at 6pm since the beginning of the week.
That would have been fine any other day up until now but they had to have a heart for me on Friday.
After CS came by the residents' workroom though and declared that it looks more like 6:30 I did go home and I'm now waiting for the page - it's 6:05pm right now.
In other news, there's nothing out of the ordinary to report for today except that I stepped out of the very boring cardiology grand rounds to go up to the residents' luncheon in A700 and didn't regret it, for after several other announcements they projected this hilarious and nerd-a-licious persiflage of a Justin Timberlake song on the silver screen as well as the three plasma panels in the room.
I'll take my gym stuff with me to the hospital later - if CS ever does page us to come.
Blog to you later.
But hey, that doesn't sound like something that could happen to me, does it? Of course not. CS had scheduled a meeting for us at 6pm since the beginning of the week.
That would have been fine any other day up until now but they had to have a heart for me on Friday.
After CS came by the residents' workroom though and declared that it looks more like 6:30 I did go home and I'm now waiting for the page - it's 6:05pm right now.
In other news, there's nothing out of the ordinary to report for today except that I stepped out of the very boring cardiology grand rounds to go up to the residents' luncheon in A700 and didn't regret it, for after several other announcements they projected this hilarious and nerd-a-licious persiflage of a Justin Timberlake song on the silver screen as well as the three plasma panels in the room.
I'll take my gym stuff with me to the hospital later - if CS ever does page us to come.
Blog to you later.
Thursday, May 3, 2007
Day three
at the new service.
Life's kind of okay.
Feet are hurting but rounds were still done at a somewhat-reasonable 6:30pm despite the attending having been in clinic again today.
The morning started slowly, after the transplant meeting at 7:30am. Yesterday I was told it would start on time, so I arrived at 7:30 sharp and naturally, I was the first one in the conference room. "On time" my behind. But they did start at 7:40. I'm not sure why I "had" to be there - I mean it was nice to see CT (cardiothoracic) surgeons are the same kind of narcissistic studs they are back in Munich. But I can't say I learned a whole lot or had anything to contribute to the mostly organizational meeting.
Anyway, after the meeting my current fellow, let's call her Jess from now on, told me that I was actually free to do what I wanted. Wow, that's new. She said I could follow up on whichever patient I wanted, she would want to teach me a thing or two about heart failure around 11:30 and there was going to be a conference on door-to-balloon-time at noon (that is in addition to the M&M meeting at the same time). Cool stuff. I could also follow the attending to clinic if I wanted but the resident was already doing that today. So I declined .. for one thing I didn't want to double-team looking over his shoulder all day plus then Jess would have no one to see new consults - should they actually come in. Which today, they would.
But first things first, around 8:30 I went up to A700 for the nice, usual Thursday ample warm cholesterol-packed breakfast. Yum. And guess who I found already sitting at a table there .. three Germans. During the course of the morning, we came and went but we still maintained a strong German presence in that room most of the time. I would have had to start getting smart about the first thing about heart failure but hey, I'm lazy and I'll prefer conversation over studying any time. So that's what I did for the following hour and a half, until morning report at 10. After a somewhat-interesting but not terribly new lecture on rhabdo I went to look at my young lawyer with the questionable sarcoidosis in his heart before going to see Jess.
As I have getting used to with my fellows, she was getting paged every five minutes while handing me and orally summarizing a few more papers. I'm not sure whether she expects me to read all this stuff any time soon or in my life, for that matter. She gave me six papers yesterday, three more today, which is in addition to the three I got from Carolin - all of these on heart failure - not even counting all the stuff from uptodate I printed on sarcoidosis (half of which I actually have read). I'm afraid this may very well turn out to be a sad waste of trees.
But interestingly, she also had two new consults. I actually had to ask whether I should see one of them and the answer was "sure, if you like". If I like? Really cool stuff. Sure I "liked" .. but then I had to choose which one. One was 77, with amyloid cardiomyopathy requiring pressors that the primary team now has trouble weaning off. The other one was 22 (!) with chest pain. Why would he be on the heart failure service? Well, because his dad knows someone that knows our attending. And as we know, our attending is good.
So I had to pick between 77-year-old guy with amyloidosis and 22-year-old with chest pain. Considering my past karma with everything I touch turning into case reports (if the biopsy's positive for sarcoidosis, we're actually going to write one) I just couldn't be responsible for this 22-year-old turning out to have some rare deadly disease. So I took the 77-year-old.
Before that though, I went up to A700 for some pizza and juicy M&M. M&Ms are usually packed, and so it was today, even though Borat was the only German I saw there. But I guess it was better that way, the place was packed despite the fact that they took out the room separator with some residents actually having to stand in the back.
After the M&M meeting, I went to see my patient. While working him up using chart and computer in the nursing station actually Jen came by. We had a nice chat, wallowing in memories of the good times we had together after having been separated for less than a week and of course making fun of the ridiculously long rounding times I was suffering from with my current attending. And following CS's suggestion, I did belatedly take her up on her offer to write an evaluation for me. Who knows, I might consider a career with the pill-pushers after all.
I just don't know anymore.
Anyway, quite a while later, at precisely 2:59pm, Jess paged me that we were "apparently" starting rounds in the ICU "now". I was at that time still extensively chatting with my new patient and his wife (attending's exuberant bedside manner already rubbing off), rushed through the exam at that point and met the team in the ICU. The attending was still discussing (what else) stuff with the ICU team, since he double-staffed as their attending as well. Meanwhile Jess was sitting at one of the computers there frantically looking up stuff on patients. She said our attending had just "dropped three more consults on her". That's not a nice thing to do minutes before rounds.
I asked her whether I could help her in any way and she declined. But having a hunch about rounds taking a while again today I sneaked out while the attending was talking to another family on the ICU down to the gift shop to get supplies (i.e. water and candy) to better make it through the rest of the day. I asked Jess and the resident whether they wanted anything and only the Indian guy accepted. I bought more though which Jess would later be grateful for after we had gone to cath the sarcoidosis suspect in the middle of rounds and her blood sugar was running low as well.
Anyway, I'll spare you the details about rounds and I'll get myself back home before it's dark again. Have been blogging for 40 minutes again. I guess I'm addicted. Will go into rehab back in good old Germany.
Oh by the way, the team is determined to take me to a karaoke place next Thursday. I'll be sure to vocally make them regret that.
Blog to you later.
Life's kind of okay.
Feet are hurting but rounds were still done at a somewhat-reasonable 6:30pm despite the attending having been in clinic again today.
The morning started slowly, after the transplant meeting at 7:30am. Yesterday I was told it would start on time, so I arrived at 7:30 sharp and naturally, I was the first one in the conference room. "On time" my behind. But they did start at 7:40. I'm not sure why I "had" to be there - I mean it was nice to see CT (cardiothoracic) surgeons are the same kind of narcissistic studs they are back in Munich. But I can't say I learned a whole lot or had anything to contribute to the mostly organizational meeting.
Anyway, after the meeting my current fellow, let's call her Jess from now on, told me that I was actually free to do what I wanted. Wow, that's new. She said I could follow up on whichever patient I wanted, she would want to teach me a thing or two about heart failure around 11:30 and there was going to be a conference on door-to-balloon-time at noon (that is in addition to the M&M meeting at the same time). Cool stuff. I could also follow the attending to clinic if I wanted but the resident was already doing that today. So I declined .. for one thing I didn't want to double-team looking over his shoulder all day plus then Jess would have no one to see new consults - should they actually come in. Which today, they would.
But first things first, around 8:30 I went up to A700 for the nice, usual Thursday ample warm cholesterol-packed breakfast. Yum. And guess who I found already sitting at a table there .. three Germans. During the course of the morning, we came and went but we still maintained a strong German presence in that room most of the time. I would have had to start getting smart about the first thing about heart failure but hey, I'm lazy and I'll prefer conversation over studying any time. So that's what I did for the following hour and a half, until morning report at 10. After a somewhat-interesting but not terribly new lecture on rhabdo I went to look at my young lawyer with the questionable sarcoidosis in his heart before going to see Jess.
As I have getting used to with my fellows, she was getting paged every five minutes while handing me and orally summarizing a few more papers. I'm not sure whether she expects me to read all this stuff any time soon or in my life, for that matter. She gave me six papers yesterday, three more today, which is in addition to the three I got from Carolin - all of these on heart failure - not even counting all the stuff from uptodate I printed on sarcoidosis (half of which I actually have read). I'm afraid this may very well turn out to be a sad waste of trees.
But interestingly, she also had two new consults. I actually had to ask whether I should see one of them and the answer was "sure, if you like". If I like? Really cool stuff. Sure I "liked" .. but then I had to choose which one. One was 77, with amyloid cardiomyopathy requiring pressors that the primary team now has trouble weaning off. The other one was 22 (!) with chest pain. Why would he be on the heart failure service? Well, because his dad knows someone that knows our attending. And as we know, our attending is good.
So I had to pick between 77-year-old guy with amyloidosis and 22-year-old with chest pain. Considering my past karma with everything I touch turning into case reports (if the biopsy's positive for sarcoidosis, we're actually going to write one) I just couldn't be responsible for this 22-year-old turning out to have some rare deadly disease. So I took the 77-year-old.
Before that though, I went up to A700 for some pizza and juicy M&M. M&Ms are usually packed, and so it was today, even though Borat was the only German I saw there. But I guess it was better that way, the place was packed despite the fact that they took out the room separator with some residents actually having to stand in the back.
After the M&M meeting, I went to see my patient. While working him up using chart and computer in the nursing station actually Jen came by. We had a nice chat, wallowing in memories of the good times we had together after having been separated for less than a week and of course making fun of the ridiculously long rounding times I was suffering from with my current attending. And following CS's suggestion, I did belatedly take her up on her offer to write an evaluation for me. Who knows, I might consider a career with the pill-pushers after all.
I just don't know anymore.
Anyway, quite a while later, at precisely 2:59pm, Jess paged me that we were "apparently" starting rounds in the ICU "now". I was at that time still extensively chatting with my new patient and his wife (attending's exuberant bedside manner already rubbing off), rushed through the exam at that point and met the team in the ICU. The attending was still discussing (what else) stuff with the ICU team, since he double-staffed as their attending as well. Meanwhile Jess was sitting at one of the computers there frantically looking up stuff on patients. She said our attending had just "dropped three more consults on her". That's not a nice thing to do minutes before rounds.
I asked her whether I could help her in any way and she declined. But having a hunch about rounds taking a while again today I sneaked out while the attending was talking to another family on the ICU down to the gift shop to get supplies (i.e. water and candy) to better make it through the rest of the day. I asked Jess and the resident whether they wanted anything and only the Indian guy accepted. I bought more though which Jess would later be grateful for after we had gone to cath the sarcoidosis suspect in the middle of rounds and her blood sugar was running low as well.
Anyway, I'll spare you the details about rounds and I'll get myself back home before it's dark again. Have been blogging for 40 minutes again. I guess I'm addicted. Will go into rehab back in good old Germany.
Oh by the way, the team is determined to take me to a karaoke place next Thursday. I'll be sure to vocally make them regret that.
Blog to you later.
Wednesday, May 2, 2007
Special touch
There seems to be another recurring theme - my very first patient on a new service apparently regularly turns out to be case report-worthy.
Remember, the patient I saw on the very first morning I started in this hospital was the deaf-mute lady that ingested 50,000 units of vitamin D per day for an entire year and came in wildly hypercalcemic.
I also told you about the young guy yesterday that could easily bench press me. Turns out, heart failure apparently was the right service for this guy after all. (Actually, general cards, electrophysiology as well as we ourselves were all consulting on this same guy.) During rounds today (that thankfully ended with only two hours of overtime), we got a call from the general cards attending that had evaluated this guy's cardiac MRI, who was apparently very excited about it. So we went to his office and had a look. He demonstrated patchy hyperintense infiltrates in the myocardium very much consistent with sarcoidosis (or maybe some other form of myocarditis). We call-conferenced with the electrophysiology attending and my current attending on the heart failure service received kudos for actually having come up with sarcoidosis on the differential in this guy even before the MRI.
So we (fellow, resident and I) had our work cut out for ourselves .. look up sarcoidosis and its manifestation in the heart till tomorrow.
So that's what I'll get started on while still here in the hospital, since I'll need access to uptodate and medical journals.
But I'm hungry, tired (got only 5 hours last night) and my feet hurt up to the knees.
Surgery suddenly looks very attractive right now. My feet are going to hurt anyway and at least I won't have to think anymore.
Blog to you later.
Remember, the patient I saw on the very first morning I started in this hospital was the deaf-mute lady that ingested 50,000 units of vitamin D per day for an entire year and came in wildly hypercalcemic.
I also told you about the young guy yesterday that could easily bench press me. Turns out, heart failure apparently was the right service for this guy after all. (Actually, general cards, electrophysiology as well as we ourselves were all consulting on this same guy.) During rounds today (that thankfully ended with only two hours of overtime), we got a call from the general cards attending that had evaluated this guy's cardiac MRI, who was apparently very excited about it. So we went to his office and had a look. He demonstrated patchy hyperintense infiltrates in the myocardium very much consistent with sarcoidosis (or maybe some other form of myocarditis). We call-conferenced with the electrophysiology attending and my current attending on the heart failure service received kudos for actually having come up with sarcoidosis on the differential in this guy even before the MRI.
So we (fellow, resident and I) had our work cut out for ourselves .. look up sarcoidosis and its manifestation in the heart till tomorrow.
So that's what I'll get started on while still here in the hospital, since I'll need access to uptodate and medical journals.
But I'm hungry, tired (got only 5 hours last night) and my feet hurt up to the knees.
Surgery suddenly looks very attractive right now. My feet are going to hurt anyway and at least I won't have to think anymore.
Blog to you later.
Tuesday, May 1, 2007
Wind of change
So, lots to tell from these past days. I'll start with the "highlights".
Yesterday was my last day of renal consults. And I actually felt sad about that. Jen asked me whether I needed an evaluation. Before I could respond by saying "no, thanks", the attending chimed in with "don't worry about that I'm on top of it". Uh-huh, I am being evaluated now? I felt tempted to ask who she was going to send that evaluation to but refrained. She said I had nothing to worry about there, I was a "ten". Uhm, OK. Now I'm hoping that's not on a scale from 1 to 100. Anyway, renal days are over. I'll miss 'em.
Today is May 1st, started on a new service. I was actually scheduled to do regular cardiology for all of May but so was another student from Germany that arrived a few days ago. That's why CS spontaneously arranged for me to go join the heart failure team, basically a different kind of cardiology service. She asked me to come to the EKG conference this morning .. at 7:45am, mind you! So I did. The conference was good, strongly reminded me of the electrolyte conferences nephrologists hold. I guess the EKG is to the cardiologist what lytes are to the nephro guy. And similarly, the conference was almost equally sophisticated.
Afterwards, CS paged the heart failure team. The fellow was a little busy .. as was to be expected on the first day on the new service. Problem was that she also just received a new resident from Boston University who didn't know the way around the hospital (later on told me he spent an hour in the morning trying to find where he was supposed to go), didn't have a pager and didn't have access to the computer systems here. So in addition to having to deal with the patient collective of a new service, she had to get this resident settled in. Naturally (from what I gathered from listening to CS's side of the conversation), she was not so happy about having to deal with a new medstudent on top of everything. Oh, by the way, Tuesday afternoon is her clinic.
That's why my new fellow said she'd meet CS and me later and CS let me go for a second breakfast after the one at the EKG conference. So I went up to A700 around 9:30am, sending a text message to one of the two new Germans that had started today that I had time to show them where they could get free breakfast. I figured they'd probably be working on getting IDs and the likes right about now. So I sent the message and went up to A700 to find all other German medstudents were already there. So I guess my work there was done. I spoke to them shortly, went to the back to get my usual bagel and orange juice, came back and they were gone. Guess they hate me or something.
Anyway, I sat down and started peeking into one of the papers on heart failure that CS had printed out for me before. Shortly thereafter though, I was relieved by the student that I'll be sharing the cardiology services with this month. He was brought back up there by his resident and told to see the "conference", meaning morning report later on. We chatted for a while until one of the chief residents called us in for morning report. The case presented was a somewhat-interesting patient CDCD (as I just learned .. circling the drain awaiting celestial discharge) whose disposition seems to have raised numerous ethical dilemmas. Before I could find out what happened to her, around 10:30am, my pager went off and Carolin asked to meet me.
She brought me in to my "new team", which was basically that fellow I told you about earlier with her new indian resident who was in bad need of some orientation and access credentials. The fellow started rotating pretty much at that point, between the signout list she had opened on her computer, talking to the new resident, receiving pages, "welcoming" me, introducing all those people around her and mentioning that she had a consult. She asked me whether I could see this patient. Now at this point I got a flashback to my very first day here. "It's kind of a crazy day, could you just go see this one?" The new fellow did not quite exhibit the same amount of grace and good humor while massively multitasking but nevertheless, the resemblance was striking.
Anyway, while she was still spinning on that chair trying to get things for the day organized she pointed to one of the nearby laptops, asking me to get started on the patient right away. So I started collecting information from the computer. About 20 minutes later, she was ready to go on what would turn out to be her own little version of rounds, including a little tour for the new guy. Which would be the resident. She rounded just with us, without the attending, because - naturally - he was in clinic. As she would be later on, which I had already mentioned. But I actually only learned these facts about halfway through the pretty small list of patients on the heart failure service. Apparently, what she was discussing with us was our preparation to round with the attending later.
Ain't that something.
The clock was advancing towards noon-ish, at which time the fellow had to leave to her clinic. She handed me a sheet listing the patients on the service, asked me to look up the serum levels of immunosuppressants on three of them and to see the new guy until "rounds". I asked when that would be and she replied it'd be whenever the attending gets out of clinic, an indefinite amount of time that he will page us at.
The resident stated he would get lunch now and started walking out the ICU in the wrong direction, so I printed out the map of the hospital that had served me so well before for him and sent him on his way to "au bon pain".
In the meantime, I would have liked to go to Grand Rounds and eat lunch but that would have meant I'm out of the game until 1pm with no idea when the attending would want to round and be presented with my first patient on this service. So I went there right away. The case was rather straightforward, what kept me busy was the fact that I had extremely negligible experience dealing with heart nuclear scans, echos and catheters, all of which this 32-year-old guy had had. But I worked through his chart and computer files in the usual manner and talked to him for quite a while afterwards. He was a nice guy. Lawyer. Tall, bulky, but lean. He bench presses 250 pounds, he told me. I wouldn't dream of that. What team am I on again? Heart failure?
I'm glad I remembered that before automatically asking him for a urine sample. Might have wanted to do a tox screen though. He sounded like an upstanding guy but his muscular shape seemed pretty borderline towards having used stuff to get a little edge in the weightlifting game.
Anyway, back to the day. I was just about done with him around 1:30pm, going back to the T elevators to go down to the lobby. I wanted to get some candy from the gift shop to make it through the day and also in order to break a $20 bill. I'd probably need $1 bills for the bus later. Because I was scheduled to meet a friend tonight. A friend who lives in Berlin that I haven't seen in many years. She was in Chicago with a friend and she would be here until tomorrow morning. The three of us had a date in the Signature Lounge on the 95th floor of the Hancock Building tonight at 7pm. Even though I'd need about an hour to get to downtown from here, I was confident that I'd make that given that I've never really had to stay longer than 6pm.
Boy, was I wrong.
Anyway, on my way to the elevators, I met the Indian resident. He expressed his relief that he had found his way back from "au bon pain" to the fifth floor, where the patients were. He seemed a bit surprised that I had seen the patient by now and said that he would have wanted to see the patient with me. So I took him back there with me. Unfortunately, the patient was about to leave for another echo (with contrast this time) and that would mean his chart goes with him. So the Indian resident and I sat down at the nurse's station, I logged in with the credentials I still have from Jen (he won't get his until at least Friday), gave him a 5-minute-crash-course on oacis and left him reading the little info on the patient there was while I headed down for candy, change and a double-chocolate muffin at "au bon pain".
Muffin in hand, I went right back up. By now, it was around 2pm. I asked the resident whether he knew when the attending would be out of clinic to round with us. He said he had heard someone say "around 3". Ouch. And I had actually been under the illusion that I'd have time to go the extra lecture on preeclampsia at 4pm in the lecture hall today that my old attending and Jen had recommended to me yesterday. If we were to start rounding at 3, that would probably not happen. But hey. This service was tiny compared to renal before.
During that time, I counted April's renal consults that were still on Jen's and my list in oacis. There were 115 patients total, 3.8 per calendar day, 5.5 per workday (which is when consults are most often called for). I saw only 25 of these patients, which works out to 1.2 per working day. I believe there were only two days in the month where I did not see a consult alone. At any one time, there would be roughly 22-30 patients on the service.
Compared to this service, which apparently actively carries 7 patients right now, plus the new one I got today that was able to bench press me lying flat on his bed (as compared to the renal patients, more than half of which were on one of the ICUs, most of those intubated).
So you'd think we would be done somewhat quickly wouldn't you.
At 2:30pm I did dare to text-page our fellow that I was done with the patient and whether there'd be anything else we should do awaiting the advent of the attending we had never seen yet. She actually called me back and said that our attending was just about to be done in clinic, I should hang on a few more minutes. After a few more minutes, I decided to go to the bathroom while the resident was hovering over the phone. When I came back, he said that the attending wanted to meet us in the echo lab. So we went there.
In the echo lab, the other cardiology team with the other German medstudent was already happily rounding along, their attending apparently teaching them intermittently on the interpretation of cardiac echos. The resident and I waited outside for ten minutes. And another ten. Around 3pm (so the prediction was going to be correct) the attending showed, with a pharmaceutical doctor in his tow. After we had gotten acquainted for about 30 seconds we went into the dark lair where echos were evaluated on screen and the attending started a discussion with the cardiologist sitting at the computer about residency programs, research, this-and-that attending and just about anything until after maybe 10 minutes we started looking at the echo of "my guy" before I had even presented his case. Didn't seem to matter much for two reasons .. one was that the attending apparently already had heard the gist about him and the second reason was that he really didn't have much on his echo. Which was good. The guy was 32 after all.
So around 3:20pm we got out of there. The attending declared that we would now have to see the transplant patients first, since that was what the pharmaceutical guy was here for. And first on the list was the 12-year-old heart-transplanted kid from Japan. 12 years, man. Myocarditis is a bitch. So we went all the way over to the children's hospital and spent the better part of the rest of the hour watching the attending while he was talking to this kid's whole family from Japan via an interpreter, examining the child and having various discussions with the huge crowd of various health care providers ranging from nurses to physicians to case managers to the pharma guy. My only contribution was the tacrolimus level for this little guy that I had looked up around lunch. It was high.
While they were still discussing, it got very close to 4pm so I found a nearby computer and text-paged Jen that I wouldn't make it to the lecture, asking her to pay extra attention for me.
Shortly after 4pm, the attending seemed satisfied for the day with the child's healthcare.
So we headed back to the adult building. We met a nurse practitioner on the way. The attending now declared that we would have to see an "NP" case now. This guy wasn't on our lists. We went up to the sixth floor to this 60-ish-year-old patient that had lost both his legs to peripheral vascular disease, had received a combined heart-kidney-pancreas transplant almost 10 (!) years ago, was now developing a squamous cell carcinoma on his neck and still came on to the female nurses and docs on this floor. Can't really blame him though because he was right, they were "lookers" as he pointed out. So after that took about another 20 minutes, we walked back to the elevators around 4:40pm. The attending looked at his watch and stated that he actually had to be interviewing someone for a job here at 4:30pm and was scheduled for a meeting with "his boss" (whoever that is) at 5pm. He was fully aware that we had seen one out of the seven patients on the list of this service and apologized, saying he was afraid this may become "a long night".
Uhm, kay.
So he took off. The resident asked me whether we should go for coffee then since it was going to be a long night. Very funny. So we went down to "au bon pain", I got a cookie with m&m's in it and a bottle of water and sat down with the Indian. We talked for a good while - about airplane companies, his family, the transplanted playa, stem cell research, abortion, religion, God until we were tired of talking. All the while, I was sending cell phone messages back and forth with the friend from Berlin that I was supposed to be meeting. At around 6pm we gave up waiting down there and went up to the residents' workroom where I had actually started this blog entry close to six hours ago.
I saw both other new Germans there who were obviously done for the day, one of them preparing something for tomorrow it seemed. CS also stopped by and I tried to tickle some sympathy out of her for the fact that the one day that I actually had some kind of social activity planned out here in over a month I would be spending a "long night" at the hospital it seemed.
And I really couldn't just go - not without presenting the patient I had seen to the attending. That's really, truly, unthinkable. Naive and optimistic as I still was (can you imagine me optimistic? I was!) I still thought I could maybe make it. Down in "au bon pain" the Indian had offered to take me downtown in his car after rounds. He would even let me change quickly at home.
So when the attending finally paged us around 6:15pm, I still had a glimmer of hope that I'd only be late for the Signature Lounge and that I'd get to see the girls before they went on through the country. The attending said we should meet him in the D5 ICU in "around 10 minutes", he was still seeing yet another patient there. The guy was seeing yet another patient that wasn't even on our list. I urged the resident to come with me to D5 right away to see what the heck was going on.
And there he was, standing amidst the on-call D5 team. One of the residents of that team had been on renal consults with me before. So in between the vivid but somewhat repetitive discussions on what to do with this patient that was CDCD I asked that resident whether they had curbsided our attending on this. He looked puzzled and replied that he was "their attending". Apparently he was double-staffing D5 and heart failure.
That's fine. There's not really much to do on the heart failure team. But at some point, you have to actually start doing it!
The attending did no such thing. As I watched the minute hand of the clock on the wall calmly tick towards 7pm, they were still talking circles around this patient's care and how they should *not* wake the attending if he coded at 4am.
After 7, the attending apologetically turned to us and declared to the ICU team that he would now have to see to it that we would get home. How nice. The problem was that by now, I had understood that this guy just doesn't do quick consults. In the subsequent rounds he did with us, he initially flipped through the charts a bit faster but other than that did not really change his pace. Thankfully the patient on ICU was intubated. For the other ones were not and boy, did this guy have time to talk to them.
I was still constantly pushing back my calculations, deciding to skip changing and having myself be driven downtown right away but it was just no use. At 7:45pm, when we still hadn't come by my own patient, I wrote to my friend that I was sorry.
And I really was. I was really looking forward to seeing her again as well as getting an excellent opportunity to see the Signature Lounge and to get out of my apartment, maybe even to find some kind of attractive side to this city.
But I guess that's Internal Medicine for you.
Talking, talking, fiddling around with numbers and medications and some more talking.
But here's the scary part. The attending did an incredible amount of talking to all of those patients. But - he did it well. I actually *liked* listening to him. He's such an example of speaking to patients on their level, comforting them with compassion and care but at the same time being absolutely but NOT brutally honest. He could relate to them, be their friend instantly yet still emanate a respectful exterior and they'd still be smiling at him and nodding when he would speak about the direst truths.
After I had given up hope on the Signature Lounge, he actually wanted to let me go at 8:30pm, right after having finally seen (and talked extensively to) my one patient for the day. But at that point a patient's daughter (of a patient we had seen right before mine) asked to talk to him. And I voluntarily stayed at that point, because I really did enjoy listening to him talk to patients. Since it was decided that my plans for the night had to be scrapped, I also went along to the follow-up on the last patient. Here, even the attending showed signs of fatigue but I still didn't regret tagging along just for hearing this guy speak to the patient.
It may be partially blamed on severe hypoglycemia on my part after having skipped lunch and dinner today but in the end I couldn't even be mad at this attending for ruining the one glimmer of a social life I was going to have here.
I'm so weak.
And right now it's ten after midnight, my blogging time is clearly feasting on my sleep and I do feel worn out and hardly able to keep my eyes open.
Good thing that I can type blindly.
Too bad that this has probably been too long for any of you to still be reading. If you are, I congratulate you. If not, I'm sure I'll be reading this myself around ten years from now. Or probably not. I'll have too many interesting new things then to spend time on I hope. If not, I'll be smiling right about now plus ten years.
Allright. That's enough. It's even clear to me now that I need to sleep. So I will. Soon. Bye.
Yesterday was my last day of renal consults. And I actually felt sad about that. Jen asked me whether I needed an evaluation. Before I could respond by saying "no, thanks", the attending chimed in with "don't worry about that I'm on top of it". Uh-huh, I am being evaluated now? I felt tempted to ask who she was going to send that evaluation to but refrained. She said I had nothing to worry about there, I was a "ten". Uhm, OK. Now I'm hoping that's not on a scale from 1 to 100. Anyway, renal days are over. I'll miss 'em.
Today is May 1st, started on a new service. I was actually scheduled to do regular cardiology for all of May but so was another student from Germany that arrived a few days ago. That's why CS spontaneously arranged for me to go join the heart failure team, basically a different kind of cardiology service. She asked me to come to the EKG conference this morning .. at 7:45am, mind you! So I did. The conference was good, strongly reminded me of the electrolyte conferences nephrologists hold. I guess the EKG is to the cardiologist what lytes are to the nephro guy. And similarly, the conference was almost equally sophisticated.
Afterwards, CS paged the heart failure team. The fellow was a little busy .. as was to be expected on the first day on the new service. Problem was that she also just received a new resident from Boston University who didn't know the way around the hospital (later on told me he spent an hour in the morning trying to find where he was supposed to go), didn't have a pager and didn't have access to the computer systems here. So in addition to having to deal with the patient collective of a new service, she had to get this resident settled in. Naturally (from what I gathered from listening to CS's side of the conversation), she was not so happy about having to deal with a new medstudent on top of everything. Oh, by the way, Tuesday afternoon is her clinic.
That's why my new fellow said she'd meet CS and me later and CS let me go for a second breakfast after the one at the EKG conference. So I went up to A700 around 9:30am, sending a text message to one of the two new Germans that had started today that I had time to show them where they could get free breakfast. I figured they'd probably be working on getting IDs and the likes right about now. So I sent the message and went up to A700 to find all other German medstudents were already there. So I guess my work there was done. I spoke to them shortly, went to the back to get my usual bagel and orange juice, came back and they were gone. Guess they hate me or something.
Anyway, I sat down and started peeking into one of the papers on heart failure that CS had printed out for me before. Shortly thereafter though, I was relieved by the student that I'll be sharing the cardiology services with this month. He was brought back up there by his resident and told to see the "conference", meaning morning report later on. We chatted for a while until one of the chief residents called us in for morning report. The case presented was a somewhat-interesting patient CDCD (as I just learned .. circling the drain awaiting celestial discharge) whose disposition seems to have raised numerous ethical dilemmas. Before I could find out what happened to her, around 10:30am, my pager went off and Carolin asked to meet me.
She brought me in to my "new team", which was basically that fellow I told you about earlier with her new indian resident who was in bad need of some orientation and access credentials. The fellow started rotating pretty much at that point, between the signout list she had opened on her computer, talking to the new resident, receiving pages, "welcoming" me, introducing all those people around her and mentioning that she had a consult. She asked me whether I could see this patient. Now at this point I got a flashback to my very first day here. "It's kind of a crazy day, could you just go see this one?" The new fellow did not quite exhibit the same amount of grace and good humor while massively multitasking but nevertheless, the resemblance was striking.
Anyway, while she was still spinning on that chair trying to get things for the day organized she pointed to one of the nearby laptops, asking me to get started on the patient right away. So I started collecting information from the computer. About 20 minutes later, she was ready to go on what would turn out to be her own little version of rounds, including a little tour for the new guy. Which would be the resident. She rounded just with us, without the attending, because - naturally - he was in clinic. As she would be later on, which I had already mentioned. But I actually only learned these facts about halfway through the pretty small list of patients on the heart failure service. Apparently, what she was discussing with us was our preparation to round with the attending later.
Ain't that something.
The clock was advancing towards noon-ish, at which time the fellow had to leave to her clinic. She handed me a sheet listing the patients on the service, asked me to look up the serum levels of immunosuppressants on three of them and to see the new guy until "rounds". I asked when that would be and she replied it'd be whenever the attending gets out of clinic, an indefinite amount of time that he will page us at.
The resident stated he would get lunch now and started walking out the ICU in the wrong direction, so I printed out the map of the hospital that had served me so well before for him and sent him on his way to "au bon pain".
In the meantime, I would have liked to go to Grand Rounds and eat lunch but that would have meant I'm out of the game until 1pm with no idea when the attending would want to round and be presented with my first patient on this service. So I went there right away. The case was rather straightforward, what kept me busy was the fact that I had extremely negligible experience dealing with heart nuclear scans, echos and catheters, all of which this 32-year-old guy had had. But I worked through his chart and computer files in the usual manner and talked to him for quite a while afterwards. He was a nice guy. Lawyer. Tall, bulky, but lean. He bench presses 250 pounds, he told me. I wouldn't dream of that. What team am I on again? Heart failure?
I'm glad I remembered that before automatically asking him for a urine sample. Might have wanted to do a tox screen though. He sounded like an upstanding guy but his muscular shape seemed pretty borderline towards having used stuff to get a little edge in the weightlifting game.
Anyway, back to the day. I was just about done with him around 1:30pm, going back to the T elevators to go down to the lobby. I wanted to get some candy from the gift shop to make it through the day and also in order to break a $20 bill. I'd probably need $1 bills for the bus later. Because I was scheduled to meet a friend tonight. A friend who lives in Berlin that I haven't seen in many years. She was in Chicago with a friend and she would be here until tomorrow morning. The three of us had a date in the Signature Lounge on the 95th floor of the Hancock Building tonight at 7pm. Even though I'd need about an hour to get to downtown from here, I was confident that I'd make that given that I've never really had to stay longer than 6pm.
Boy, was I wrong.
Anyway, on my way to the elevators, I met the Indian resident. He expressed his relief that he had found his way back from "au bon pain" to the fifth floor, where the patients were. He seemed a bit surprised that I had seen the patient by now and said that he would have wanted to see the patient with me. So I took him back there with me. Unfortunately, the patient was about to leave for another echo (with contrast this time) and that would mean his chart goes with him. So the Indian resident and I sat down at the nurse's station, I logged in with the credentials I still have from Jen (he won't get his until at least Friday), gave him a 5-minute-crash-course on oacis and left him reading the little info on the patient there was while I headed down for candy, change and a double-chocolate muffin at "au bon pain".
Muffin in hand, I went right back up. By now, it was around 2pm. I asked the resident whether he knew when the attending would be out of clinic to round with us. He said he had heard someone say "around 3". Ouch. And I had actually been under the illusion that I'd have time to go the extra lecture on preeclampsia at 4pm in the lecture hall today that my old attending and Jen had recommended to me yesterday. If we were to start rounding at 3, that would probably not happen. But hey. This service was tiny compared to renal before.
During that time, I counted April's renal consults that were still on Jen's and my list in oacis. There were 115 patients total, 3.8 per calendar day, 5.5 per workday (which is when consults are most often called for). I saw only 25 of these patients, which works out to 1.2 per working day. I believe there were only two days in the month where I did not see a consult alone. At any one time, there would be roughly 22-30 patients on the service.
Compared to this service, which apparently actively carries 7 patients right now, plus the new one I got today that was able to bench press me lying flat on his bed (as compared to the renal patients, more than half of which were on one of the ICUs, most of those intubated).
So you'd think we would be done somewhat quickly wouldn't you.
At 2:30pm I did dare to text-page our fellow that I was done with the patient and whether there'd be anything else we should do awaiting the advent of the attending we had never seen yet. She actually called me back and said that our attending was just about to be done in clinic, I should hang on a few more minutes. After a few more minutes, I decided to go to the bathroom while the resident was hovering over the phone. When I came back, he said that the attending wanted to meet us in the echo lab. So we went there.
In the echo lab, the other cardiology team with the other German medstudent was already happily rounding along, their attending apparently teaching them intermittently on the interpretation of cardiac echos. The resident and I waited outside for ten minutes. And another ten. Around 3pm (so the prediction was going to be correct) the attending showed, with a pharmaceutical doctor in his tow. After we had gotten acquainted for about 30 seconds we went into the dark lair where echos were evaluated on screen and the attending started a discussion with the cardiologist sitting at the computer about residency programs, research, this-and-that attending and just about anything until after maybe 10 minutes we started looking at the echo of "my guy" before I had even presented his case. Didn't seem to matter much for two reasons .. one was that the attending apparently already had heard the gist about him and the second reason was that he really didn't have much on his echo. Which was good. The guy was 32 after all.
So around 3:20pm we got out of there. The attending declared that we would now have to see the transplant patients first, since that was what the pharmaceutical guy was here for. And first on the list was the 12-year-old heart-transplanted kid from Japan. 12 years, man. Myocarditis is a bitch. So we went all the way over to the children's hospital and spent the better part of the rest of the hour watching the attending while he was talking to this kid's whole family from Japan via an interpreter, examining the child and having various discussions with the huge crowd of various health care providers ranging from nurses to physicians to case managers to the pharma guy. My only contribution was the tacrolimus level for this little guy that I had looked up around lunch. It was high.
While they were still discussing, it got very close to 4pm so I found a nearby computer and text-paged Jen that I wouldn't make it to the lecture, asking her to pay extra attention for me.
Shortly after 4pm, the attending seemed satisfied for the day with the child's healthcare.
So we headed back to the adult building. We met a nurse practitioner on the way. The attending now declared that we would have to see an "NP" case now. This guy wasn't on our lists. We went up to the sixth floor to this 60-ish-year-old patient that had lost both his legs to peripheral vascular disease, had received a combined heart-kidney-pancreas transplant almost 10 (!) years ago, was now developing a squamous cell carcinoma on his neck and still came on to the female nurses and docs on this floor. Can't really blame him though because he was right, they were "lookers" as he pointed out. So after that took about another 20 minutes, we walked back to the elevators around 4:40pm. The attending looked at his watch and stated that he actually had to be interviewing someone for a job here at 4:30pm and was scheduled for a meeting with "his boss" (whoever that is) at 5pm. He was fully aware that we had seen one out of the seven patients on the list of this service and apologized, saying he was afraid this may become "a long night".
Uhm, kay.
So he took off. The resident asked me whether we should go for coffee then since it was going to be a long night. Very funny. So we went down to "au bon pain", I got a cookie with m&m's in it and a bottle of water and sat down with the Indian. We talked for a good while - about airplane companies, his family, the transplanted playa, stem cell research, abortion, religion, God until we were tired of talking. All the while, I was sending cell phone messages back and forth with the friend from Berlin that I was supposed to be meeting. At around 6pm we gave up waiting down there and went up to the residents' workroom where I had actually started this blog entry close to six hours ago.
I saw both other new Germans there who were obviously done for the day, one of them preparing something for tomorrow it seemed. CS also stopped by and I tried to tickle some sympathy out of her for the fact that the one day that I actually had some kind of social activity planned out here in over a month I would be spending a "long night" at the hospital it seemed.
And I really couldn't just go - not without presenting the patient I had seen to the attending. That's really, truly, unthinkable. Naive and optimistic as I still was (can you imagine me optimistic? I was!) I still thought I could maybe make it. Down in "au bon pain" the Indian had offered to take me downtown in his car after rounds. He would even let me change quickly at home.
So when the attending finally paged us around 6:15pm, I still had a glimmer of hope that I'd only be late for the Signature Lounge and that I'd get to see the girls before they went on through the country. The attending said we should meet him in the D5 ICU in "around 10 minutes", he was still seeing yet another patient there. The guy was seeing yet another patient that wasn't even on our list. I urged the resident to come with me to D5 right away to see what the heck was going on.
And there he was, standing amidst the on-call D5 team. One of the residents of that team had been on renal consults with me before. So in between the vivid but somewhat repetitive discussions on what to do with this patient that was CDCD I asked that resident whether they had curbsided our attending on this. He looked puzzled and replied that he was "their attending". Apparently he was double-staffing D5 and heart failure.
That's fine. There's not really much to do on the heart failure team. But at some point, you have to actually start doing it!
The attending did no such thing. As I watched the minute hand of the clock on the wall calmly tick towards 7pm, they were still talking circles around this patient's care and how they should *not* wake the attending if he coded at 4am.
After 7, the attending apologetically turned to us and declared to the ICU team that he would now have to see to it that we would get home. How nice. The problem was that by now, I had understood that this guy just doesn't do quick consults. In the subsequent rounds he did with us, he initially flipped through the charts a bit faster but other than that did not really change his pace. Thankfully the patient on ICU was intubated. For the other ones were not and boy, did this guy have time to talk to them.
I was still constantly pushing back my calculations, deciding to skip changing and having myself be driven downtown right away but it was just no use. At 7:45pm, when we still hadn't come by my own patient, I wrote to my friend that I was sorry.
And I really was. I was really looking forward to seeing her again as well as getting an excellent opportunity to see the Signature Lounge and to get out of my apartment, maybe even to find some kind of attractive side to this city.
But I guess that's Internal Medicine for you.
Talking, talking, fiddling around with numbers and medications and some more talking.
But here's the scary part. The attending did an incredible amount of talking to all of those patients. But - he did it well. I actually *liked* listening to him. He's such an example of speaking to patients on their level, comforting them with compassion and care but at the same time being absolutely but NOT brutally honest. He could relate to them, be their friend instantly yet still emanate a respectful exterior and they'd still be smiling at him and nodding when he would speak about the direst truths.
After I had given up hope on the Signature Lounge, he actually wanted to let me go at 8:30pm, right after having finally seen (and talked extensively to) my one patient for the day. But at that point a patient's daughter (of a patient we had seen right before mine) asked to talk to him. And I voluntarily stayed at that point, because I really did enjoy listening to him talk to patients. Since it was decided that my plans for the night had to be scrapped, I also went along to the follow-up on the last patient. Here, even the attending showed signs of fatigue but I still didn't regret tagging along just for hearing this guy speak to the patient.
It may be partially blamed on severe hypoglycemia on my part after having skipped lunch and dinner today but in the end I couldn't even be mad at this attending for ruining the one glimmer of a social life I was going to have here.
I'm so weak.
And right now it's ten after midnight, my blogging time is clearly feasting on my sleep and I do feel worn out and hardly able to keep my eyes open.
Good thing that I can type blindly.
Too bad that this has probably been too long for any of you to still be reading. If you are, I congratulate you. If not, I'm sure I'll be reading this myself around ten years from now. Or probably not. I'll have too many interesting new things then to spend time on I hope. If not, I'll be smiling right about now plus ten years.
Allright. That's enough. It's even clear to me now that I need to sleep. So I will. Soon. Bye.
Saturday, April 28, 2007
"Ummm, I'm thinking about math."
That was the answer from the guy on "my" team when I asked him what his major was. He was a first year college student.
Then those kids started kicking my ass on the basketball court again.
I'm old.
Then those kids started kicking my ass on the basketball court again.
I'm old.
Wednesday, April 25, 2007
Oh!
And looking at the post below I just realized that I forgot to tell you what prompted the post's title .. "routine".
I meant to tell you that I finally had a routine down in the morning, going up to A700 in the morning after having thrown my jacket into the residents' workroom, picking up the current list of patients on the consult service in the dialysis unit on the way, then paging Jen from one of the phones in the kitchen, putting a halved bagel into the toaster, pouring orange juice into a cup, at which point Jen will return the page, I talk to her, after which the bagel is done and I put some toppings on it, after which I go sit down at a computer and check up on old patients in the computer or, if I'm lazier than that, I'll just check my mail, read the news or start blogging.
I did the latter today, but was rudely interrupted by the first later-to-be-cancelled consult in mid-breakfast as you can read in the post below.
Blog to you later!
I meant to tell you that I finally had a routine down in the morning, going up to A700 in the morning after having thrown my jacket into the residents' workroom, picking up the current list of patients on the consult service in the dialysis unit on the way, then paging Jen from one of the phones in the kitchen, putting a halved bagel into the toaster, pouring orange juice into a cup, at which point Jen will return the page, I talk to her, after which the bagel is done and I put some toppings on it, after which I go sit down at a computer and check up on old patients in the computer or, if I'm lazier than that, I'll just check my mail, read the news or start blogging.
I did the latter today, but was rudely interrupted by the first later-to-be-cancelled consult in mid-breakfast as you can read in the post below.
Blog to you later!
Routine
Yesterday, the service was back up to its usual five consults. Most notable exception was that my patient for the day was in the ER again, a place I still like to go to. Although I'm far from being an expert yet, nephrology is already becoming a bit monotonous. If I imagine focusing on the kidney for a significant number of years, like my attending would approve, it doesn't seem like that could still be interesting then. And I don't feel like one has to be particularly smart to do it. There's a large but still limited number of diseases a kidney can have and it still holds true that hearing hooves usually signifies horses. And figuring out the occasional zebra will certainly be satisfying but rare (and we're here at a good university hospital in a consult service that deals with the cases the primary teams cannot or will not figure out - so pretty selected collective of patients already). I'd still rather be in the ER, obviously things were less repetitive in there.
That said, it's not completely boring here. Physicians mix things up by overdosing people on Lasix last night, for example, poor guy's in the ICU and probably deaf right about now. I guess I shouldn't go into details on that.
And another interesting mix-up happened .. apparently someone was very much post-call and wrote an order for DDAVP (desmopressin, basically vasopressin with an arginine attached) for a patient with a sodium of 120. Apparently they got it confused with another medication starting with "D": Demeclocycline, a vasopressin antagonist, after having been awake for too long. I guess we're all human.
(Disclaimer: These stories are needless to say purely fictional and any resemblance to actual events or persons is, of course, coincidental.)
(I started this post with breakfast in the morning. This is the third time I was interrupted and I'm continuing this draft, it's 7:30pm and I'm back home.)
So, where was I. Ah well, what does it matter anyway.
The reason I was interrupted so often today was that the two residents we had up until yesterday were done with their renal consults. We got one new resident today, but she was, of course, in clinic this morning. That left Jen and myself, Jen having a kidney biopsy scheduled. That's how I ended up with my first consult at 8:45am, when I had spent one and a half hours on it and was close to getting done she paged me again to let me know the primary team had just cancelled the consult. They'd send the patient home this afternoon. 20 minutes later I got another patient, HIV+ with PCP in the MICU. 33 minutes later, at 11:07am (I'm reconstructing this from my pager) Jen called again to inform me she was about to start the biopsy and given that this had taken more than an hour yesterday she would like me to get started on a third patient. I replied "Sure. So you're planning on rounding around 5pm, right?". I was trying to make sense of this guy in the MICU's chart again but failed miserably. He had apparently been turfed from one place to the next a lot, hitting one normal ward, one step-down service and three different ICUs in little more than a week. Naturally, they all had different kinds of flow sheets that overlapped (good luck trying to figure out ins and outs there) and medication orders were a mess.
To paint you a picture: One and the same medication, Bactrim, was showing up on the same day's medication sheet three times. Once as p.o. medication, with a "d/c'd" behind it, as in "discontinued". One more line saying "Bactrim", this time i.v. and with some number of mg/kg but no times of administration behind it. And a third line on that same page starting with "Bactrim", i.v. again, this time saying 250mg and followed by four different times of administration. Two of those time points were circled, two were crossed out, all carried some hieroglyphs around them - presumably initials from nurses but they could mean anything as long as you're not familiar with *all* of the abbreviations that could be used on these medication order sheets. It turns out that the circled times of administration are doses that are not actually given to the patient, while the crossed out ones are. And that's only one of the four different antibiotics this person has been given in the time he was there, not even speaking of the plethora of other medication this 69 y/o HIV, HepC, PCP, HTN, CRI now septic patient has been given over the past week. It took me probably about five minutes of deciphering interns', residents' and especially surgeons handwriting just to find out when the guy was intubated - namely yesterday.
I would have needed a very high threshold for frustration today, which, alas, I didn't have. It was frustrating that it still takes me forever to assemble the simplest pieces of information and I'm still not sure how I can speed it up.
The best way probably is to keep doing consults. Although it probably wouldn't hurt if someone at some point sat down with me and gave me an introduction into things like "a circle around a time point on the MAR record means that this dose was actually not given". Thank you, you've just saved me half an hour of grief and the recorded fluid intake on the flow sheet finally goes together with the fact that this antibiotic is administered in 500ml IVPBs.
You live, you learn.
That said, it's not completely boring here. Physicians mix things up by overdosing people on Lasix last night, for example, poor guy's in the ICU and probably deaf right about now. I guess I shouldn't go into details on that.
And another interesting mix-up happened .. apparently someone was very much post-call and wrote an order for DDAVP (desmopressin, basically vasopressin with an arginine attached) for a patient with a sodium of 120. Apparently they got it confused with another medication starting with "D": Demeclocycline, a vasopressin antagonist, after having been awake for too long. I guess we're all human.
(Disclaimer: These stories are needless to say purely fictional and any resemblance to actual events or persons is, of course, coincidental.)
(I started this post with breakfast in the morning. This is the third time I was interrupted and I'm continuing this draft, it's 7:30pm and I'm back home.)
So, where was I. Ah well, what does it matter anyway.
The reason I was interrupted so often today was that the two residents we had up until yesterday were done with their renal consults. We got one new resident today, but she was, of course, in clinic this morning. That left Jen and myself, Jen having a kidney biopsy scheduled. That's how I ended up with my first consult at 8:45am, when I had spent one and a half hours on it and was close to getting done she paged me again to let me know the primary team had just cancelled the consult. They'd send the patient home this afternoon. 20 minutes later I got another patient, HIV+ with PCP in the MICU. 33 minutes later, at 11:07am (I'm reconstructing this from my pager) Jen called again to inform me she was about to start the biopsy and given that this had taken more than an hour yesterday she would like me to get started on a third patient. I replied "Sure. So you're planning on rounding around 5pm, right?". I was trying to make sense of this guy in the MICU's chart again but failed miserably. He had apparently been turfed from one place to the next a lot, hitting one normal ward, one step-down service and three different ICUs in little more than a week. Naturally, they all had different kinds of flow sheets that overlapped (good luck trying to figure out ins and outs there) and medication orders were a mess.
To paint you a picture: One and the same medication, Bactrim, was showing up on the same day's medication sheet three times. Once as p.o. medication, with a "d/c'd" behind it, as in "discontinued". One more line saying "Bactrim", this time i.v. and with some number of mg/kg but no times of administration behind it. And a third line on that same page starting with "Bactrim", i.v. again, this time saying 250mg and followed by four different times of administration. Two of those time points were circled, two were crossed out, all carried some hieroglyphs around them - presumably initials from nurses but they could mean anything as long as you're not familiar with *all* of the abbreviations that could be used on these medication order sheets. It turns out that the circled times of administration are doses that are not actually given to the patient, while the crossed out ones are. And that's only one of the four different antibiotics this person has been given in the time he was there, not even speaking of the plethora of other medication this 69 y/o HIV, HepC, PCP, HTN, CRI now septic patient has been given over the past week. It took me probably about five minutes of deciphering interns', residents' and especially surgeons handwriting just to find out when the guy was intubated - namely yesterday.
I would have needed a very high threshold for frustration today, which, alas, I didn't have. It was frustrating that it still takes me forever to assemble the simplest pieces of information and I'm still not sure how I can speed it up.
The best way probably is to keep doing consults. Although it probably wouldn't hurt if someone at some point sat down with me and gave me an introduction into things like "a circle around a time point on the MAR record means that this dose was actually not given". Thank you, you've just saved me half an hour of grief and the recorded fluid intake on the flow sheet finally goes together with the fact that this antibiotic is administered in 500ml IVPBs.
You live, you learn.
Monday, April 23, 2007
Day off
Wow .. just one single little consult for the entire service today. And since I checked in after one of the residents this morning, he got it and I didn't even have to do it. Now I know what hem/onc service must feel like ;D
I had time for morning report as well as electrolyte conference today. I'm going to miss the latter next month. The attending - or should I say guru - at the head of the table has an extremely calm and wise aura about him as he infers incredible amounts of information from little more than about a dozen lab values and how they develop over time. Actually, the fellows go through the labs, commenting them, and the attending - who never heard about the case before either - asks questions. Questions like (I'm just making these up for illustration, don't even have a clue whether they make sense) "so, what would give you a urine osmolality this high with a TTKG (trans-tubular potassium gradient) of 5 in the setting of severe dehydration?" Or "what's the mechanism of renal failure in severe hypercalcemia with non-gap acidosis?" Uh, well, uhm .. luckily the fellows react similarly often enough, which makes it even more humbling and awesome when this attending kindly and most of all vividly describes (or leads us on the way of finding ourselves) the pathophysiology behind everything.
Yes, you read right. Physiology. This man does care about mere ions and ion channels and enzymes and pathways yet manages to not only integrate all that knowledge into an astoundingly accurate clinical picture of the patient (without history, physical exam or any other information, just part of their labs over one or two weeks!) but he also describes them as entertainingly and plastically as only Americans can. It's like a German professor in pathophysiology crossed with an American teacher.
He's awesome.
If my kidneys ever get sick, I'd rather have this man take a look at my labs for one minute than 10 other docs conferring for hours.
Oh, and I believe I had already mentioned that the pizza is good.
I had time for morning report as well as electrolyte conference today. I'm going to miss the latter next month. The attending - or should I say guru - at the head of the table has an extremely calm and wise aura about him as he infers incredible amounts of information from little more than about a dozen lab values and how they develop over time. Actually, the fellows go through the labs, commenting them, and the attending - who never heard about the case before either - asks questions. Questions like (I'm just making these up for illustration, don't even have a clue whether they make sense) "so, what would give you a urine osmolality this high with a TTKG (trans-tubular potassium gradient) of 5 in the setting of severe dehydration?" Or "what's the mechanism of renal failure in severe hypercalcemia with non-gap acidosis?" Uh, well, uhm .. luckily the fellows react similarly often enough, which makes it even more humbling and awesome when this attending kindly and most of all vividly describes (or leads us on the way of finding ourselves) the pathophysiology behind everything.
Yes, you read right. Physiology. This man does care about mere ions and ion channels and enzymes and pathways yet manages to not only integrate all that knowledge into an astoundingly accurate clinical picture of the patient (without history, physical exam or any other information, just part of their labs over one or two weeks!) but he also describes them as entertainingly and plastically as only Americans can. It's like a German professor in pathophysiology crossed with an American teacher.
He's awesome.
If my kidneys ever get sick, I'd rather have this man take a look at my labs for one minute than 10 other docs conferring for hours.
Oh, and I believe I had already mentioned that the pizza is good.
Sunday, April 22, 2007
Lake Michigan
Hello reader,
another little picture post.
I didn't find out the weather was so beautiful yesterday until I stepped outside on the way to the library. It was surprisingly warm again and I was wearing way too many clothes. Then again, I thought the library would probably be air-conditioned. Because I actually went to the library, shortly. It was pretty much deserted as it has been the only other time I had been there. Interestingly, their first floor is open 24/7 for your studying needs - and so far hardly anyone is in that huge, endless library even during the day. So I decided I wouldn't be in there either, took my stuff and left, riding my beach cruiser bike east and further east
and further east still going
still going east on 55th (can you feel the tension rising?)
east on 55th (can you feel the tension rising?) crossed the metra tracks (almost there!), look to the sidewalk on the right to get an indication of the temperature yesterday
crossed the metra tracks (almost there!), look to the sidewalk on the right to get an indication of the temperature yesterday
 and boom!
and boom! The lake.
The lake. With a mild breeze and plenty of sunshine.
With a mild breeze and plenty of sunshine. I sat down at the tip of the headland up there and got my book out. Took me about 20 seconds to get distracted not by these guys
I sat down at the tip of the headland up there and got my book out. Took me about 20 seconds to get distracted not by these guys and not the view
and not the view but those three people in the middle, walking away.
but those three people in the middle, walking away. The two people on the right are married and from Finland, with him doing an internship with a law firm and her doing research in pharmacoeconomics here. The girl on the left is actually from Germany and also doing an internship in the law firm. They were here to kill time waiting for their tickets to Body Worlds that they had bought at 10am to become valid at 6:15pm. Apparently they sold tickets for the same day at that place that would make people wait more than eight hours to get in. Well, as you probably know any excuse is good enough for me when it comes to not having to study, so I talked to them.
The two people on the right are married and from Finland, with him doing an internship with a law firm and her doing research in pharmacoeconomics here. The girl on the left is actually from Germany and also doing an internship in the law firm. They were here to kill time waiting for their tickets to Body Worlds that they had bought at 10am to become valid at 6:15pm. Apparently they sold tickets for the same day at that place that would make people wait more than eight hours to get in. Well, as you probably know any excuse is good enough for me when it comes to not having to study, so I talked to them.
another little picture post.
I didn't find out the weather was so beautiful yesterday until I stepped outside on the way to the library. It was surprisingly warm again and I was wearing way too many clothes. Then again, I thought the library would probably be air-conditioned. Because I actually went to the library, shortly. It was pretty much deserted as it has been the only other time I had been there. Interestingly, their first floor is open 24/7 for your studying needs - and so far hardly anyone is in that huge, endless library even during the day. So I decided I wouldn't be in there either, took my stuff and left, riding my beach cruiser bike east
 and further east
and further east still going
still going east on 55th (can you feel the tension rising?)
east on 55th (can you feel the tension rising?) crossed the metra tracks (almost there!), look to the sidewalk on the right to get an indication of the temperature yesterday
crossed the metra tracks (almost there!), look to the sidewalk on the right to get an indication of the temperature yesterday and boom!
and boom! The lake.
The lake. With a mild breeze and plenty of sunshine.
With a mild breeze and plenty of sunshine. I sat down at the tip of the headland up there and got my book out. Took me about 20 seconds to get distracted not by these guys
I sat down at the tip of the headland up there and got my book out. Took me about 20 seconds to get distracted not by these guys and not the view
and not the view but those three people in the middle, walking away.
but those three people in the middle, walking away. The two people on the right are married and from Finland, with him doing an internship with a law firm and her doing research in pharmacoeconomics here. The girl on the left is actually from Germany and also doing an internship in the law firm. They were here to kill time waiting for their tickets to Body Worlds that they had bought at 10am to become valid at 6:15pm. Apparently they sold tickets for the same day at that place that would make people wait more than eight hours to get in. Well, as you probably know any excuse is good enough for me when it comes to not having to study, so I talked to them.
The two people on the right are married and from Finland, with him doing an internship with a law firm and her doing research in pharmacoeconomics here. The girl on the left is actually from Germany and also doing an internship in the law firm. They were here to kill time waiting for their tickets to Body Worlds that they had bought at 10am to become valid at 6:15pm. Apparently they sold tickets for the same day at that place that would make people wait more than eight hours to get in. Well, as you probably know any excuse is good enough for me when it comes to not having to study, so I talked to them.
Saturday, April 21, 2007
A day at the U of C
Hello, reader.
As per popular request, this will be a picture post. You're right, my past posts have been .. shall we say biased towards text. So I took the camera with me on Thursday - and you'll have the questionable pleasure of following me along on that day. There'll be huge gaps in between - that's when I either felt I shouldn't be pointing my camera at people or when I simply forgot to take pictures.
Here we go.
At around 7:30, I got out of bed, which looks somewhat like this.
 As anyone who knows me will be aware, my first order of business is switching on my computer - yes, the thing in the middle of the mess on my desk.
As anyone who knows me will be aware, my first order of business is switching on my computer - yes, the thing in the middle of the mess on my desk. After checking my mail in the morning, which usually isn't much given that people in Germany are usually still at work at this time, I visit my beautiful bathroom.
After checking my mail in the morning, which usually isn't much given that people in Germany are usually still at work at this time, I visit my beautiful bathroom. After about 1 minute to shave, 30 seconds for the hair, two minutes for my teeth and 15 minutes for my tie I look somewhat like this.
After about 1 minute to shave, 30 seconds for the hair, two minutes for my teeth and 15 minutes for my tie I look somewhat like this. Notice the camera bag on the right, that baby is coming with me today.
Notice the camera bag on the right, that baby is coming with me today.
Out the door and to the left, we're heading down the corridor to the stairs
to the stairs through this door into the laundry room
through this door into the laundry room to find my beautiful bike.
to find my beautiful bike. Can you see it? You should know what it looks like by now!
Can you see it? You should know what it looks like by now!
Well, I found it and with it, I headed out. Three doors later, which I'm actually not going to show you, we hit this fence. After having overcome even this obstacle, we go down the driveway,
After having overcome even this obstacle, we go down the driveway, Make a right onto this little street, glancing at Ratner's across the intersection, (yes! This part of the story is very detailed!)
Make a right onto this little street, glancing at Ratner's across the intersection, (yes! This part of the story is very detailed!) carefully making sure there's no police cars when I fail to stop at every friggin' stop sign around here before making a left at this intersection.
carefully making sure there's no police cars when I fail to stop at every friggin' stop sign around here before making a left at this intersection. One left turn later, we go straight ahead across 55th street (the red lights seem to be another suggestion to stop around here, how anyone gets from A to B here is beyond me).
One left turn later, we go straight ahead across 55th street (the red lights seem to be another suggestion to stop around here, how anyone gets from A to B here is beyond me). Look at that! There actually was a police car across the street there.
Look at that! There actually was a police car across the street there.
We're on Ellis Avenue now, going south - in case you'd like to know so you can follow along on Google Earth. Quite exciting, isn't it. Here we are, merrily whistling a song while going south on Ellis.
Here we are, merrily whistling a song while going south on Ellis. We wave at that nuclear thingy, before pretending to stop at yet another stop sign and making a right turn onto 57th.
We wave at that nuclear thingy, before pretending to stop at yet another stop sign and making a right turn onto 57th. After that turn, we find yet another stop sign. By the way, that pedestrian crossing connects Crerar library on the left to the Pritzker med school building on the right. Isn't that interesting.
After that turn, we find yet another stop sign. By the way, that pedestrian crossing connects Crerar library on the left to the Pritzker med school building on the right. Isn't that interesting.
 Next stop sign - let's make a left here. It'd really be shorter to go one more block ahead and then turn left but hey, I'm taking the scenic route for you guys.
Next stop sign - let's make a left here. It'd really be shorter to go one more block ahead and then turn left but hey, I'm taking the scenic route for you guys. We're getting closer .. look to the right.
We're getting closer .. look to the right. At the end of this street, right where it says "Adult Emergency", we turn right.
At the end of this street, right where it says "Adult Emergency", we turn right. There we are .. "The University of Chicago Hospitals".
There we are .. "The University of Chicago Hospitals". Let's make a sharp right in front of the new Duchossois Center
Let's make a sharp right in front of the new Duchossois Center and park our vehicle.
and park our vehicle. Turn around - and there it is.
Turn around - and there it is. Mitchell Hospital. Where I'm going to be for the next 10 hours.
Mitchell Hospital. Where I'm going to be for the next 10 hours. It must have been around 8:30am by now. It was Thursday, which meant Jen would be in clinic all morning. That's not a good thing. By now, we actually had two residents on the service. Interestingly, both were post-call this morning. That means they have spent the night here and courtesy demands they should be let go as quickly as possible, usually until noon.
It must have been around 8:30am by now. It was Thursday, which meant Jen would be in clinic all morning. That's not a good thing. By now, we actually had two residents on the service. Interestingly, both were post-call this morning. That means they have spent the night here and courtesy demands they should be let go as quickly as possible, usually until noon.
That was semi-good for me, it meant that the residents would get the very first consults this morning and I could go have breakfast.
So I entered the hospital through the lobby and went on through
and went on through to the "T" elevators.
to the "T" elevators. These elevators actually have three cars but sometimes you're just out of luck and they're not coming by any time soon.
These elevators actually have three cars but sometimes you're just out of luck and they're not coming by any time soon.
So I took the stairs up to the fifth floor.
up to the fifth floor. My first stop as every morning is the residents' workroom.
My first stop as every morning is the residents' workroom.
You can actually see the door, it's the first one on the left in the corridor ahead.
This is where I leave my jacket during the day. But we said breakfast, right? Right! So we leave the workroom and navigate towards A700.
But we said breakfast, right? Right! So we leave the workroom and navigate towards A700. You are going to see parts of the way there, I took a picture whenever there wasn't anyone coming the other way.
You are going to see parts of the way there, I took a picture whenever there wasn't anyone coming the other way.
I went down the D corridor, past the Clinical Research Center (this is a place where they emulate any kinds of conditions they need for patients enrolled in studies. For example, there was "wake at 7:06am" written on one of the doors. I fought the urge to knock on it, heheh). But today, I walked past the CRC in the W corridor and continued straight ahead - the D corridor is from here on called M corridor. And no, there is absolutely no logic behind the naming of corridors here. The whole complex has been designed to get you lost.
and continued straight ahead - the D corridor is from here on called M corridor. And no, there is absolutely no logic behind the naming of corridors here. The whole complex has been designed to get you lost. After I made a right at the next intersection - you'd expect to be in a corridor with a different letter. And that's true most of the time - except M (as well as at least C, D and W) is an exception here. I made a right, yet I was still in the M corridor. I'm telling you - if you're there for the first time without a map you will not find anything by yourself. Nothing.
After I made a right at the next intersection - you'd expect to be in a corridor with a different letter. And that's true most of the time - except M (as well as at least C, D and W) is an exception here. I made a right, yet I was still in the M corridor. I'm telling you - if you're there for the first time without a map you will not find anything by yourself. Nothing.
Strolling down the M corridor, I saw a familiar face. After confirming with Borat that there'd still be food for me upstairs I continued on merrily.
After confirming with Borat that there'd still be food for me upstairs I continued on merrily. A left at this intersection brings us to the A corridor! Hooray!
A left at this intersection brings us to the A corridor! Hooray!
So all we need to do is go two floors up. And we're here!
And we're here!
There's "hot" breakfast on Thursdays, so it's a good idea to be there rather early (as opposed to 10am with morning report). There's "breakfast pizzas" in here. I'm sure that sounds like a strange idea to some of you - but as you can probably imagine, I can eat anything at any time of day, and I like pizza.
There's "breakfast pizzas" in here. I'm sure that sounds like a strange idea to some of you - but as you can probably imagine, I can eat anything at any time of day, and I like pizza. In the back, around the corner, where the "cold" regular breakfast usually is, beverages await.
In the back, around the corner, where the "cold" regular breakfast usually is, beverages await. And there you go, a nice, fresh, warm, cholesterol-binge breakfast to start off a beautiful day.
And there you go, a nice, fresh, warm, cholesterol-binge breakfast to start off a beautiful day. Sooner or later, I would have to inform Jen that I was here though, so I paged her.
Sooner or later, I would have to inform Jen that I was here though, so I paged her. She called back and said - as expected - she didn't have anything for me yet. And actually, one of the residents was up there in A700 with me, so he hadn't been sent out yet either.
She called back and said - as expected - she didn't have anything for me yet. And actually, one of the residents was up there in A700 with me, so he hadn't been sent out yet either.
But this was actually rather normal. The primary teams get around to calling consults only after they're done rounding in the morning. That's usually not until 9:30 or so.
That meant, I had time to check labs and imaging studies on my old patients. So I sat down at one of the computers up there and had a look around in oacis, their clinical data software. Not too long though, since as expected, Jen chimed in around 9:30.
Not too long though, since as expected, Jen chimed in around 9:30. 65 year old female with protein and blood in her urine for over a week. Jen gave me the parts of the story that the resident on the primary team had relayed to her and off I went to 5NE (five-north-east) in the main building.
65 year old female with protein and blood in her urine for over a week. Jen gave me the parts of the story that the resident on the primary team had relayed to her and off I went to 5NE (five-north-east) in the main building.
Down the stairs This time I chose to take the W corridor, so straight ahead past dialysis and the urine room (don't worry .. you'll get to see that later ..)
This time I chose to take the W corridor, so straight ahead past dialysis and the urine room (don't worry .. you'll get to see that later ..) Back into the D corridor
Back into the D corridor past the ICUs (there's a different ICU on every floor in the D building, or rather the "Rubloff ICU Tower")
past the ICUs (there's a different ICU on every floor in the D building, or rather the "Rubloff ICU Tower")
 and on towards the Mitchell main building.
and on towards the Mitchell main building. We're heading north here and if I make a right turn behind these doors, we will be in 5NE.
We're heading north here and if I make a right turn behind these doors, we will be in 5NE. An example of what I could have found out about this lady is on the picture below.
An example of what I could have found out about this lady is on the picture below.
Naturally, I cannot divulge any information about my actual patients, so the information in that picture is purely fictional and written down by me as an example template. Any resemblance to persons, living or dead, is of course purely coincidental.
Click on the picture to magnify. I spent about two hours on this consult, including actually talking to the patient, physical exam and acquiring the patient's urine. I spent most of the time rummaging around nurses' and physicians' notes and deciphering handwriting since I was interested in the time course of this lady's surgery, hematuria, foley placement and antibiotic administration - which of course had to be reconstructed from clues hidden around the chart.
I spent about two hours on this consult, including actually talking to the patient, physical exam and acquiring the patient's urine. I spent most of the time rummaging around nurses' and physicians' notes and deciphering handwriting since I was interested in the time course of this lady's surgery, hematuria, foley placement and antibiotic administration - which of course had to be reconstructed from clues hidden around the chart.
So around 11:30am, I went on my way all the way back to the W corridor (I'll spare you the way there this time) and entered the urine room.
Ta-daaa! Yucky, isn't it.
Yucky, isn't it.
Before I could dip the urine and spin it down, the pager went off again. Jen again. Uh-oh.
Jen again. Uh-oh. Next consult. Patient with questionable altered mental status. Oh, and she doesn't speak English, only Spanish. Yay.
Next consult. Patient with questionable altered mental status. Oh, and she doesn't speak English, only Spanish. Yay.
Jen also told me that we'd try to get together to round around 2pm.
After I was done dipping the urine and looking at the sediment, it was almost noon.
and looking at the sediment, it was almost noon.
I decided that I'd have lunch despite the consult and went up to A700. And at the prospect of food I actually forgot to take any pictures of it. Sorry. It was good though. About 15 minutes later, I went to see that other patient.
 While I was starting to look if I could find anything that would correlate severe iron overload with renal failure, I was interrupted by the pager again.
While I was starting to look if I could find anything that would correlate severe iron overload with renal failure, I was interrupted by the pager again.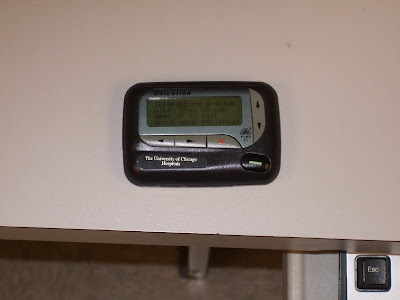 OK fine, no looking things up yet again.
OK fine, no looking things up yet again.
Jen wanted to meet soon, so I had to go spin down this patient's urine now.
After all three of us (residents were at home by now) had looked at today's urines, we unanimously decided to sit down in the nephrology conference room to discuss the new patients. This is the conference room with Jen and the attending trying to find the stuff they'd need to make coffee.
This is the conference room with Jen and the attending trying to find the stuff they'd need to make coffee. After that, there's not much more to show. After Jen and I had presented our patients to the attending, we went on to see them all (6 today, three seen by the two residents, two by me and one Jen managed after clinic) plus the old ones. When they offered for me to leave at around six, they were not done rounding yet.
After that, there's not much more to show. After Jen and I had presented our patients to the attending, we went on to see them all (6 today, three seen by the two residents, two by me and one Jen managed after clinic) plus the old ones. When they offered for me to leave at around six, they were not done rounding yet.
I got some bad news from Trillian, so I went home quickly to talk to her.
I needed water (still not convinced to drink the tap water here that has so much chlorine that showering reminds me of a swimming pool), so I went grocery shopping afterwards and brought back another two gallons. They last for about three days, at least my fluid intake seems to be good enough.
Anyway, that was my day, hope you had enough pictures to last you a while. Next post will contain pictures as well, though.
Blog to you later.
As per popular request, this will be a picture post. You're right, my past posts have been .. shall we say biased towards text. So I took the camera with me on Thursday - and you'll have the questionable pleasure of following me along on that day. There'll be huge gaps in between - that's when I either felt I shouldn't be pointing my camera at people or when I simply forgot to take pictures.
Here we go.
At around 7:30, I got out of bed, which looks somewhat like this.
 As anyone who knows me will be aware, my first order of business is switching on my computer - yes, the thing in the middle of the mess on my desk.
As anyone who knows me will be aware, my first order of business is switching on my computer - yes, the thing in the middle of the mess on my desk. After checking my mail in the morning, which usually isn't much given that people in Germany are usually still at work at this time, I visit my beautiful bathroom.
After checking my mail in the morning, which usually isn't much given that people in Germany are usually still at work at this time, I visit my beautiful bathroom. After about 1 minute to shave, 30 seconds for the hair, two minutes for my teeth and 15 minutes for my tie I look somewhat like this.
After about 1 minute to shave, 30 seconds for the hair, two minutes for my teeth and 15 minutes for my tie I look somewhat like this. Notice the camera bag on the right, that baby is coming with me today.
Notice the camera bag on the right, that baby is coming with me today.Out the door and to the left, we're heading down the corridor
 to the stairs
to the stairs through this door into the laundry room
through this door into the laundry room to find my beautiful bike.
to find my beautiful bike. Can you see it? You should know what it looks like by now!
Can you see it? You should know what it looks like by now!Well, I found it and with it, I headed out. Three doors later, which I'm actually not going to show you, we hit this fence.
 After having overcome even this obstacle, we go down the driveway,
After having overcome even this obstacle, we go down the driveway, Make a right onto this little street, glancing at Ratner's across the intersection, (yes! This part of the story is very detailed!)
Make a right onto this little street, glancing at Ratner's across the intersection, (yes! This part of the story is very detailed!) carefully making sure there's no police cars when I fail to stop at every friggin' stop sign around here before making a left at this intersection.
carefully making sure there's no police cars when I fail to stop at every friggin' stop sign around here before making a left at this intersection. One left turn later, we go straight ahead across 55th street (the red lights seem to be another suggestion to stop around here, how anyone gets from A to B here is beyond me).
One left turn later, we go straight ahead across 55th street (the red lights seem to be another suggestion to stop around here, how anyone gets from A to B here is beyond me). Look at that! There actually was a police car across the street there.
Look at that! There actually was a police car across the street there.We're on Ellis Avenue now, going south - in case you'd like to know so you can follow along on Google Earth. Quite exciting, isn't it.
 Here we are, merrily whistling a song while going south on Ellis.
Here we are, merrily whistling a song while going south on Ellis. We wave at that nuclear thingy, before pretending to stop at yet another stop sign and making a right turn onto 57th.
We wave at that nuclear thingy, before pretending to stop at yet another stop sign and making a right turn onto 57th. After that turn, we find yet another stop sign. By the way, that pedestrian crossing connects Crerar library on the left to the Pritzker med school building on the right. Isn't that interesting.
After that turn, we find yet another stop sign. By the way, that pedestrian crossing connects Crerar library on the left to the Pritzker med school building on the right. Isn't that interesting. Next stop sign - let's make a left here. It'd really be shorter to go one more block ahead and then turn left but hey, I'm taking the scenic route for you guys.
Next stop sign - let's make a left here. It'd really be shorter to go one more block ahead and then turn left but hey, I'm taking the scenic route for you guys. We're getting closer .. look to the right.
We're getting closer .. look to the right. At the end of this street, right where it says "Adult Emergency", we turn right.
At the end of this street, right where it says "Adult Emergency", we turn right. There we are .. "The University of Chicago Hospitals".
There we are .. "The University of Chicago Hospitals". Let's make a sharp right in front of the new Duchossois Center
Let's make a sharp right in front of the new Duchossois Center and park our vehicle.
and park our vehicle. Turn around - and there it is.
Turn around - and there it is. Mitchell Hospital. Where I'm going to be for the next 10 hours.
Mitchell Hospital. Where I'm going to be for the next 10 hours. It must have been around 8:30am by now. It was Thursday, which meant Jen would be in clinic all morning. That's not a good thing. By now, we actually had two residents on the service. Interestingly, both were post-call this morning. That means they have spent the night here and courtesy demands they should be let go as quickly as possible, usually until noon.
It must have been around 8:30am by now. It was Thursday, which meant Jen would be in clinic all morning. That's not a good thing. By now, we actually had two residents on the service. Interestingly, both were post-call this morning. That means they have spent the night here and courtesy demands they should be let go as quickly as possible, usually until noon.That was semi-good for me, it meant that the residents would get the very first consults this morning and I could go have breakfast.
So I entered the hospital through the lobby
 and went on through
and went on through to the "T" elevators.
to the "T" elevators. These elevators actually have three cars but sometimes you're just out of luck and they're not coming by any time soon.
These elevators actually have three cars but sometimes you're just out of luck and they're not coming by any time soon.So I took the stairs
 up to the fifth floor.
up to the fifth floor. My first stop as every morning is the residents' workroom.
My first stop as every morning is the residents' workroom.You can actually see the door, it's the first one on the left in the corridor ahead.
This is where I leave my jacket during the day.
 But we said breakfast, right? Right! So we leave the workroom and navigate towards A700.
But we said breakfast, right? Right! So we leave the workroom and navigate towards A700. You are going to see parts of the way there, I took a picture whenever there wasn't anyone coming the other way.
You are going to see parts of the way there, I took a picture whenever there wasn't anyone coming the other way.I went down the D corridor, past the Clinical Research Center (this is a place where they emulate any kinds of conditions they need for patients enrolled in studies. For example, there was "wake at 7:06am" written on one of the doors. I fought the urge to knock on it, heheh). But today, I walked past the CRC in the W corridor
 and continued straight ahead - the D corridor is from here on called M corridor. And no, there is absolutely no logic behind the naming of corridors here. The whole complex has been designed to get you lost.
and continued straight ahead - the D corridor is from here on called M corridor. And no, there is absolutely no logic behind the naming of corridors here. The whole complex has been designed to get you lost. After I made a right at the next intersection - you'd expect to be in a corridor with a different letter. And that's true most of the time - except M (as well as at least C, D and W) is an exception here. I made a right, yet I was still in the M corridor. I'm telling you - if you're there for the first time without a map you will not find anything by yourself. Nothing.
After I made a right at the next intersection - you'd expect to be in a corridor with a different letter. And that's true most of the time - except M (as well as at least C, D and W) is an exception here. I made a right, yet I was still in the M corridor. I'm telling you - if you're there for the first time without a map you will not find anything by yourself. Nothing.Strolling down the M corridor, I saw a familiar face.
 After confirming with Borat that there'd still be food for me upstairs I continued on merrily.
After confirming with Borat that there'd still be food for me upstairs I continued on merrily. A left at this intersection brings us to the A corridor! Hooray!
A left at this intersection brings us to the A corridor! Hooray!So all we need to do is go two floors up.
 And we're here!
And we're here!There's "hot" breakfast on Thursdays, so it's a good idea to be there rather early (as opposed to 10am with morning report).
 There's "breakfast pizzas" in here. I'm sure that sounds like a strange idea to some of you - but as you can probably imagine, I can eat anything at any time of day, and I like pizza.
There's "breakfast pizzas" in here. I'm sure that sounds like a strange idea to some of you - but as you can probably imagine, I can eat anything at any time of day, and I like pizza. In the back, around the corner, where the "cold" regular breakfast usually is, beverages await.
In the back, around the corner, where the "cold" regular breakfast usually is, beverages await. And there you go, a nice, fresh, warm, cholesterol-binge breakfast to start off a beautiful day.
And there you go, a nice, fresh, warm, cholesterol-binge breakfast to start off a beautiful day. Sooner or later, I would have to inform Jen that I was here though, so I paged her.
Sooner or later, I would have to inform Jen that I was here though, so I paged her. She called back and said - as expected - she didn't have anything for me yet. And actually, one of the residents was up there in A700 with me, so he hadn't been sent out yet either.
She called back and said - as expected - she didn't have anything for me yet. And actually, one of the residents was up there in A700 with me, so he hadn't been sent out yet either.But this was actually rather normal. The primary teams get around to calling consults only after they're done rounding in the morning. That's usually not until 9:30 or so.
That meant, I had time to check labs and imaging studies on my old patients. So I sat down at one of the computers up there and had a look around in oacis, their clinical data software.
 Not too long though, since as expected, Jen chimed in around 9:30.
Not too long though, since as expected, Jen chimed in around 9:30. 65 year old female with protein and blood in her urine for over a week. Jen gave me the parts of the story that the resident on the primary team had relayed to her and off I went to 5NE (five-north-east) in the main building.
65 year old female with protein and blood in her urine for over a week. Jen gave me the parts of the story that the resident on the primary team had relayed to her and off I went to 5NE (five-north-east) in the main building.Down the stairs
 This time I chose to take the W corridor, so straight ahead past dialysis and the urine room (don't worry .. you'll get to see that later ..)
This time I chose to take the W corridor, so straight ahead past dialysis and the urine room (don't worry .. you'll get to see that later ..) Back into the D corridor
Back into the D corridor past the ICUs (there's a different ICU on every floor in the D building, or rather the "Rubloff ICU Tower")
past the ICUs (there's a different ICU on every floor in the D building, or rather the "Rubloff ICU Tower") and on towards the Mitchell main building.
and on towards the Mitchell main building. We're heading north here and if I make a right turn behind these doors, we will be in 5NE.
We're heading north here and if I make a right turn behind these doors, we will be in 5NE. An example of what I could have found out about this lady is on the picture below.
An example of what I could have found out about this lady is on the picture below.Naturally, I cannot divulge any information about my actual patients, so the information in that picture is purely fictional and written down by me as an example template. Any resemblance to persons, living or dead, is of course purely coincidental.
Click on the picture to magnify.
 I spent about two hours on this consult, including actually talking to the patient, physical exam and acquiring the patient's urine. I spent most of the time rummaging around nurses' and physicians' notes and deciphering handwriting since I was interested in the time course of this lady's surgery, hematuria, foley placement and antibiotic administration - which of course had to be reconstructed from clues hidden around the chart.
I spent about two hours on this consult, including actually talking to the patient, physical exam and acquiring the patient's urine. I spent most of the time rummaging around nurses' and physicians' notes and deciphering handwriting since I was interested in the time course of this lady's surgery, hematuria, foley placement and antibiotic administration - which of course had to be reconstructed from clues hidden around the chart.So around 11:30am, I went on my way all the way back to the W corridor (I'll spare you the way there this time) and entered the urine room.
Ta-daaa!
 Yucky, isn't it.
Yucky, isn't it.Before I could dip the urine and spin it down, the pager went off again.
 Jen again. Uh-oh.
Jen again. Uh-oh. Next consult. Patient with questionable altered mental status. Oh, and she doesn't speak English, only Spanish. Yay.
Next consult. Patient with questionable altered mental status. Oh, and she doesn't speak English, only Spanish. Yay.Jen also told me that we'd try to get together to round around 2pm.
After I was done dipping the urine
 and looking at the sediment, it was almost noon.
and looking at the sediment, it was almost noon.I decided that I'd have lunch despite the consult and went up to A700. And at the prospect of food I actually forgot to take any pictures of it. Sorry. It was good though. About 15 minutes later, I went to see that other patient.

 While I was starting to look if I could find anything that would correlate severe iron overload with renal failure, I was interrupted by the pager again.
While I was starting to look if I could find anything that would correlate severe iron overload with renal failure, I was interrupted by the pager again. OK fine, no looking things up yet again.
OK fine, no looking things up yet again.Jen wanted to meet soon, so I had to go spin down this patient's urine now.
After all three of us (residents were at home by now) had looked at today's urines, we unanimously decided to sit down in the nephrology conference room to discuss the new patients.
 This is the conference room with Jen and the attending trying to find the stuff they'd need to make coffee.
This is the conference room with Jen and the attending trying to find the stuff they'd need to make coffee. After that, there's not much more to show. After Jen and I had presented our patients to the attending, we went on to see them all (6 today, three seen by the two residents, two by me and one Jen managed after clinic) plus the old ones. When they offered for me to leave at around six, they were not done rounding yet.
After that, there's not much more to show. After Jen and I had presented our patients to the attending, we went on to see them all (6 today, three seen by the two residents, two by me and one Jen managed after clinic) plus the old ones. When they offered for me to leave at around six, they were not done rounding yet.I got some bad news from Trillian, so I went home quickly to talk to her.
I needed water (still not convinced to drink the tap water here that has so much chlorine that showering reminds me of a swimming pool), so I went grocery shopping afterwards and brought back another two gallons. They last for about three days, at least my fluid intake seems to be good enough.
Anyway, that was my day, hope you had enough pictures to last you a while. Next post will contain pictures as well, though.
Blog to you later.
Subscribe to:
Posts (Atom)
